Translate this page into:
Knowledge, Attitudes, and Practices of Urban Workers toward Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome: Results from a Cross-sectional Study in Lubumbashi, Democratic Republic of the Congo

*Corresponding author: Olivier Mukuku, Department of Maternal and Child Health, Institut Supérieur des Techniques Médicales de Lubumbashi, Lubumbashi, Democratic Republic of the Congo. oliviermukuku@yahoo.fr
-
Received: ,
Accepted: ,
How to cite this article: Katabwa JK, Mukuku O, Wembonyama SO. Knowledge, attitudes, and practices of urban workers toward human immunodeficiency virus/acquired immunodeficiency syndrome: Re sults from a cross-sectional study in Lubumbashi, Democratic Republic of the Congo. Glob J Med Pharm Biomed Update 2022;17:4.
Abstract
Objective:
This study aims to describe knowledge, attitudes, and practices about human immunodeficiency virus/ acquired immunodeficiency syndrome (HIV/AIDS) among a sample of 563 urban workers in Lubumbashi, in the Democratic Republic of the Congo.
Material and Methods:
This was a cross-sectional study where workers’ knowledge of HIV/AIDS was measured through a French adaptation of the Brief HIV Knowledge Questionnaire.
Results:
Overall, the level of knowledge of participating workers was poor (81.9%). Working in a private company (adjusted odds ratio [aOR] = 2.0 [1.2–3.3]) and having previously tested for HIV/AIDS (aOR = 2.5 [1.5–4.3]) were associated with good knowledge level about HIV/AIDS.
Conclusion:
Our results highlight the importance of implementing different awareness and education strategies for workers.
Keywords
Human immunodeficiency virus
Acquired immunodeficiency syndrome
Knowledge
Attitude
Practice
Brief HIV knowledge questionnaire
Adults
Workers
Lubumbashi
INTRODUCTION
Discovered in the United States in 1983,[1] the human immunodeficiency virus (HIV) is one of the world’s greatest killers. According to the World Health Organization, HIV remains a major global public health problem, with nearly 33 million deaths so far. However, through improved access to effective prevention, diagnosis, treatment and care, including for opportunistic infections, HIV infection has become a chronic disease that can be managed, ensuring a long and healthy life for people living with HIV/AIDS (PLWHA).[2] Sub-Saharan Africa, the global epicenter of the acquired immunodeficiency syndrome (AIDS) pandemic, still hosts more than two-thirds of PLWHAs, with a high prevalence among adults aged 15–49 years.[3]
More than 83% of all new infections in many African countries are among young, productive people, with more women than men. Sub-Saharan Africa, with approximately 22.5 million PLWHAs and 1.3 million new infections per year, is the most affected region in the world.[4] In 2019, in the Democratic Republic of the Congo (DRC), estimates from the National Multisectoral Program to Fight AIDS (PNMLS) recorded 450,000 PLWHAs.[5]
As a result of the lack of curative treatment and an effective vaccine against HIV infection, the fight is based on information, education, and communication aimed at changing the behavior of individuals. The previous studies in Africa[6,7] have shown an increase in knowledge and positive changes in attitudes toward HIV/AIDS. On the other hand, in the DRC, according to the Demographic and Health Survey, although almost the entire population reported having heard of HIV/AIDS, only 19% of women and 29% of men aged 15–49 years have a knowledge of it that is considered to be “in-depth.”[8] It is recognized that a poor level of knowledge leads to an increase in risk behaviors.[9]
Affecting the workforce, HIV/AIDS is a serious problem in the workplace. The latter provides immense human resources for HIV prevention in a cost-effective manner and can play a key role in preventing the spread of the disease. The social and economic impact of HIV/AIDS is intensified by the fact that it mainly affects young and middle-aged adults who are in their peak years of productivity and reproduction.[10]
As HIV/AIDS is a chronic disease, sick workers are likely to become less productive and absent at work.[11] Hence, this study is important in promoting HIV/AIDS awareness and evaluating key prevention strategies. Yet no studies have been done to explore the level of knowledge, attitudes, and behaviors of workers in our community. Therefore, this study, the first of its kind, aims to describe the state of knowledge, attitudes, and practices regarding HIV/AIDS infection among urban workers in Lubumbashi, DRC.
MATERIAL AND METHODS
An analytical cross-sectional study was carried out on a sample of urban workers from public and private enterprises in Lubumbashi city, in DRC. To be eligible for this study, only workers from public and private companies were selected. In July 2021, 600 urban workers from different companies in Lubumbashi were asked by the investigators to complete a questionnaire to measure their knowledge, attitudes, and practices regarding HIV/AIDS. After explaining the purpose of the study to obtain free and informed consent, workers who agreed to participate in the study completed a questionnaire with questions about their level of knowledge about HIV/AIDS. The participants’ knowledge level was objectively measured using the Brief HIV Knowledge Questionnaire (HIV-KQ-18).[12,13] This validated scale has 18 items (“true”/“false”/“I do not know”) and obtaining a total score is possible by adding the points obtained from each question (1 point for each correct answer, 0 for a wrong answer, or for “I don’t know”). The questions focused on various items related to prevention, modes of transmission, and the evolution of the disease. The scores extend from 0 to 18 and a higher score indicates a higher knowledge level. The threshold from which a score was considered to mark a level of knowledge was set at ≤13/18.[14] The French version of this instrument was made and validated by Labra et al.[13]
Attitudes toward HIV/AIDS infection were measured through five items using the 3-point Likert scale with the following assertions: “I disagree,” “I am neutral,” and “I agree.” For HIV/AIDS practices, four items were used.
No compensatory allowance has been provided for the participation of workers in this research. This study was approved by the Medical Ethics Committee of the University of Lubumbashi.
Descriptive statistics were compiled to provide a portrait of participants’ socio-demographic characteristics, knowledge level, attitudes, and practices for HIV/AIDS. The mean HIV-KQ-18 scores and the proportion of participants with a poor knowledge level (score ≤13 out of 18) were also calculated and compared according to various subgroups of participants, using the Pearson Chi-square test in bivariate and multivariate analyzes. A multivariate logistic regression model was designed to identify the characteristics of participants associated with a good knowledge level about HIV/AIDS. The use of a multivariate model allowed for the interrelationships between the various independent variables to be taken into account and the place of certain predictors to be isolated (minimizing confusion bias). All statistical analyzes were performed using STATA 16 software and the statistical significance threshold used was 0.05.
RESULTS
A total of 563 out of 600 workers agreed to participate in the present study and complete the questionnaire, which corresponds to a participation rate of 93.8%. The socio-demographic characteristics of the participants are presented in [Table 1]. The mean age of the participating workers was 41.2 ± 13.7 years and the majority of them were men (63.2%). More than half (53.8%) of the participants were working in a private company. More than 60% (362/563) of the respondents had a university degree and 60% were married. As for religion, 40% were Catholic and 32% were Pentecostal.
| Variable | Number (n=563) | Percentage |
|---|---|---|
| Age (years) | ||
| <30 | 146 | 25.9 |
| 30–39 | 139 | 24.7 |
| 40–49 | 114 | 20.2 |
| 50–59 | 82 | 14.6 |
| ≥60 | 82 | 14.6 |
| Mean (standard deviation) | 41.2 | (13.7) |
| Gender | ||
| Male | 356 | 63.2 |
| Female | 207 | 36.8 |
| Marital status | ||
| Married | 338 | 60.0 |
| Single | 190 | 33.8 |
| Widowed | 27 | 4.8 |
| Divorced | 8 | 1.4 |
| Educational level | ||
| Primary | 31 | 5.5 |
| Secondary | 170 | 30.2 |
| Higher/University | 362 | 64.3 |
| Type of company | ||
| Private | 303 | 53.8 |
| Public | 260 | 46.2 |
| Religion | ||
| Catholic | 225 | 40.0 |
| Pentecostal | 180 | 32.0 |
| None | 33 | 5.9 |
| Muslim | 24 | 4.2 |
| Others | 101 | 17.9 |
[Table 2] presents the responses of participants to the 18 items of the HIV-KQ-18 questionnaire on knowledge about HIV/AIDS. The mean total score for HIV-KQ-18 was 10.7 ± 3.1 (range: 0 and 18). A total of 18.1% of respondents scored >13 out of 18, indicating a good level of knowledge.
| Items | True | False | I don’t know |
|---|---|---|---|
| 1. Coughing and sneezing DO not spread HIV | 18.8 | 73.2 | 8.0 |
| 2. A person can get HIV by sharing a glass of water with someone who has HIV | 9.2 | 84.4 | 6.4 |
| 3. Pulling out the penis before a man climaxes/cums keeps a woman from getting HIV during sex | 18.3 | 56.5 | 25.2 |
| 4. A woman can get HIV if she has anal sex with a man | 74.8 | 10.3 | 14.9 |
| 5. Showering, or washing one’s genitals/private parts, after sex keeps a person from getting HIV | 5.3 | 83.7 | 11.0 |
| 6. All pregnant women infected with HIV will have babies born with AIDS | 21.8 | 58.3 | 19.9 |
| 7. People who have been infected with HIV quickly show serious signs of being infected | 17.3 | 70.3 | 12.4 |
| 8. There is a vaccine that can stop adults from getting HIV | 2.3 | 67.7 | 30.0 |
| 9. People are likely to get HIV by deep kissing, putting their tongue in their partner’s mouth, if their partner has HIV | 65.9 | 20.8 | 13.3 |
| 10. A woman cannot get HIV if she has sex during her period | 7.8 | 54.7 | 37.5 |
| 11. There is a female condom that can help decrease a woman’s chance of getting HIV | 80.5 | 6.0 | 13.5 |
| 12. A natural skin condom works better against HIV than does a latex condom | 11.2 | 11.5 | 77.3 |
| 13. A person will NOT get HIV if she or he is taking antibiotics | 3.9 | 81.4 | 14.7 |
| 14. Having sex with more than one partner can increase a person’s chance of being infected with HIV | 89.4 | 7.6 | 3.0 |
| 15. Taking a test for HIV 1 week after having sex will tell a person if she or he has HIV | 25.2 | 38.5 | 36.2 |
| 16. A person can get HIV by sitting in a hot tub or a swimming pool with a person who has HIV | 25.2 | 38.5 | 36.2 |
| 17. A person can get HIV from oral sex | 3.9 | 86.2 | 9.9 |
| 18. Using Vaseline or baby oil with condoms lowers the chance of getting HIV | 69.6 | 14.0 | 16.4 |
| Mean (standard deviation) | 10.7±3.1 (range: 0–18) | ||
Of the participants, 83.5% considered HIV/AIDS to be a very worrying problem and concerned them, 84.9% said that HIV/AIDS could affect everyone, 78.7% thought that someone who buys or has a condom with him behaved badly, 82.4% agreed to voluntary HIV/AIDS testing and 87.4% disagreed that someone living with HIV/AIDS should be excluded at work [Figure 1]. In terms of practices, only 14.0% (79/563) of the respondents had used a condom at their last sexual intercourse, 40% had already obtained a condom at least once, 50.4% had already been tested for HIV/AIDS, and 32.1% had already attended a health center for HIV/AIDS information [Figure 2]. [Table 3] shows the distribution of respondents based on reasons for condom not being used in recent reports. The main reasons were fidelity (39.67%), partner refusal (19.4%), abstinence (13.6%), and decreased pleasure (9.7%).
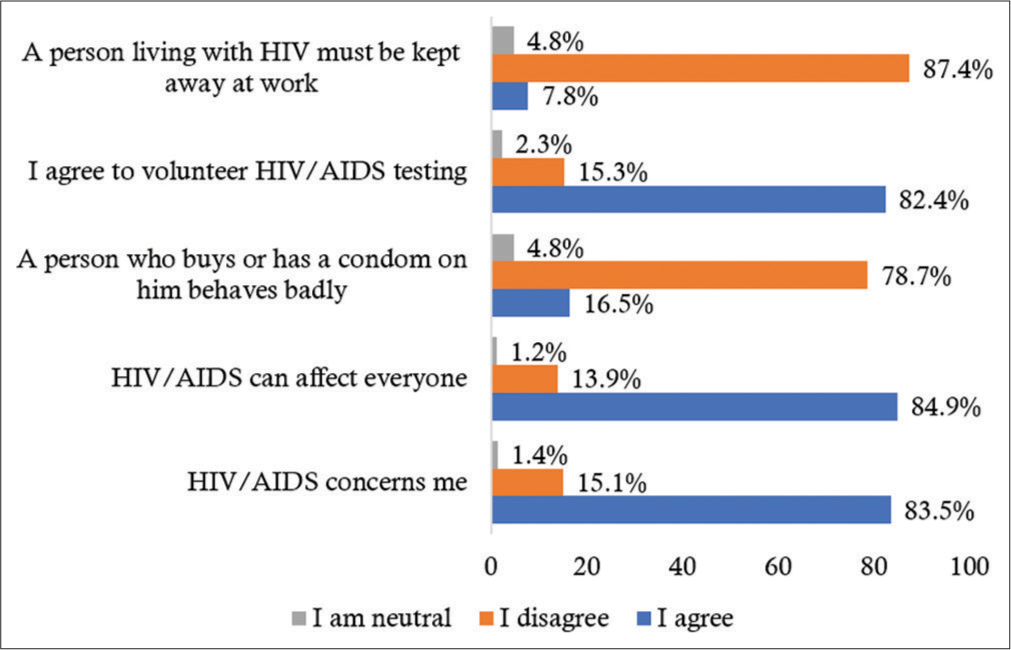
- Attitudes toward human immunodeficiency virus/ acquired immunodeficiency syndrome among 563 urban workers in Lubumbashi, Democratic Republic of the Congo.
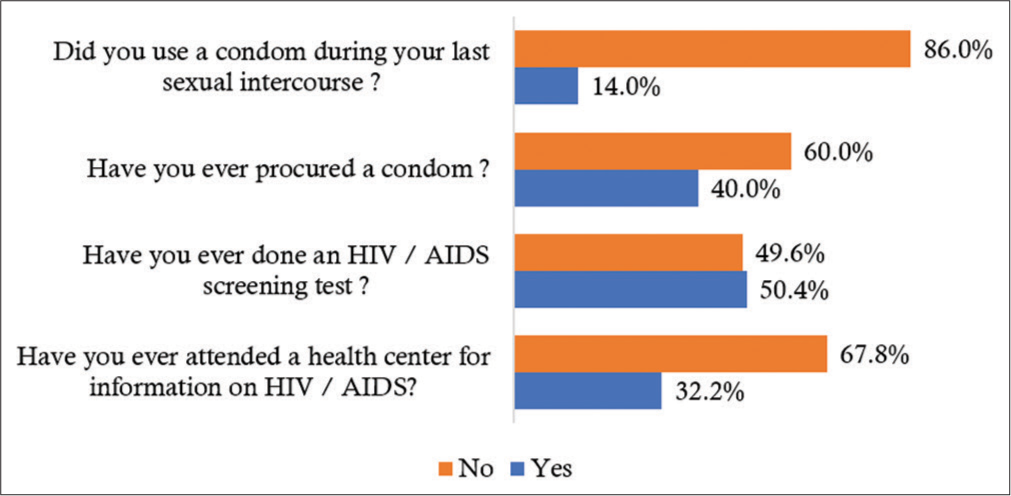
- Practices toward human immunodeficiency virus/ acquired immunodeficiency syndrome among 563 urban workers in Lubumbashi, Democratic Republic of the Congo.
| Reason | Number (n=484) | Percentage |
|---|---|---|
| Fidelity | 192 | 39.7 |
| Partner refusal | 94 | 19.4 |
| Abstinence | 66 | 13.6 |
| Decreased pleasure | 47 | 9.7 |
| No reason | 44 | 9.1 |
| Forgotten | 22 | 4.6 |
| Religious conviction | 11 | 2.3 |
| Condom not available | 8 | 1.7 |
[Table 4] shows the predictors of knowledge level for HIV/AIDS among urban workers in Lubumbashi (in DRC). Working in a private company (adjusted odds ratio [aOR] = 2.0 [1.2–3.3]) and having previously tested for HIV/AIDS (aOR = 2.5 [1.5–4.3]) were associated with a good level of knowledge about HIV/AIDS.
| Variable | Knowledge level | Crude OR (95% CI) | P-value | Adjusted OR (95% CI) | P-value | |
|---|---|---|---|---|---|---|
| Good (n=102),n (%) |
Poor (n=461),n(%) |
|||||
| Age (years) | ||||||
| <30 | 26 (17.8) | 120 (82.2) | 1.0 | 1.0 | ||
| 30–39 | 28 (20.1) | 111 (79.9) | 1.2 (0.6–2.1) | 0.725 | 1.3 (0.6–2.6) | 0.498 |
| 40–49 | 24 (21.1) | 90 (78.9) | 1.2 (0.7–2.3) | 0.617 | 1.8 (0.7–4.5) | 0.191 |
| 50–59 | 12 (14.6) | 70 (85.4) | 0.8 (0.4–1.7) | 0.665 | 1.3 (0.5–3.6) | 0.617 |
| ≥60 | 12 (14.6) | 70 (85.4) | 0.8 (0.4–1.7) | 0.665 | 1.4 (0.5–4.2) | 0.544 |
| Gender | ||||||
| Female | 41 (19.8) | 166 (80.2) | 1.0 | 1.0 | ||
| Male | 61 (17.1) | 295 (82.9) | 0.8 (0.5–1.3) | 0.496 | 0.8 (0.5–1.4) | 0.509 |
| Marital status | ||||||
| Married | 61 (18.1) | 277 (81.9) | 1.0 | 1.0 | ||
| Single | 38 (20.0) | 152 (80.0) | 1.1 (0.7–1.8) | 0.663 | 1.4 (0.7–2.8) | 0.358 |
| Widowed/Divorced | 3 (8.6) | 32 (91.4) | 0.4 (0.1–1.4) | 0.238 | 0.6 (0.2–2.4) | 0.522 |
| Educational level | ||||||
| Primary | 5 (16.1) | 26 (83.9) | 1.0 | 1.0 | ||
| Secondary | 11 (6.5) | 159 (93.5) | 0.4 (0.1–1.1) | 0.143 | 0.4 (0.1–1.1) | 0.082 |
| Higher/University | 86 (23.8) | 276 (76.2) | 1.6 (0.6–4.3) | 0.456 | 1.4 (0.5–3.8) | 0.533 |
| Religion | ||||||
| Catholic | 38 (16.9) | 187 (83.1) | 1.0 | 1.0 | ||
| Pentecostal | 33 (18.3) | 147 (81.7) | 1.1 (0.7–1.8) | 0.804 | 1.2 (0.7–2.0) | 0.583 |
| None | 4 (16.7) | 20 (83.3) | 1.0 (0.2–3.2) | 1.000 | 1.5 (05–5.1) | 0.501 |
| Muslim | 27 (20.2) | 107 (79.8) | 1.2 (0.7–2.1) | 0.526 | 1.6 (0.9–2.8) | 0,267 |
| Type of company | ||||||
| Public | 35 (13.5) | 225 (86.5) | 1.0 | 1.0 | ||
| Private | 67 (22.1) | 236 (77.9) | 1.8 (1.2–2.9) | 0.008 | 2.0 (1.2–3.3) | 0.010 |
| Have ever visited a health center on HIV/AIDS information | ||||||
| Yes | 40 (22.1) | 141 (77.9) | 1.5 (0.9–2.3) | 0.116 | 1.1 (0.7–1.8) | 0.790 |
| No | 62 (16.2) | 320 (83.8) | 1.0 | 1.0 | ||
| Have ever done an HIV/AIDS screening test | ||||||
| Yes | 72 (25.4) | 212 (74.6) | 2.8 (1.8–4.5) | 0.000 | 2.5 (1.5–4.3) | 0.001 |
| No | 30 (10.8) | 249 (89.2) | 1.0 | 1.0 | ||
DISCUSSION
The present study provides access to valuable data about the knowledge, attitudes, and practices among urban workers in Lubumbashi (in the DRC). When asked about participants’ level of knowledge, the results showed that it was poor (81.9%). This poor level of knowledge translates into a high number of bad beliefs (misconceptions) among participants. For example, a number of respondents believed that coughing or sneezing can transmit HIV (18.8%), that all HIV-infected pregnant women will give birth to an HIV-infected child (16.5%), that people are at risk of HIV infection when they hug and kiss an HIV-infected partner (21.8%) intensely/with their tongue, that people who are HIV-infected quickly show serious signs and symptoms of infection (70.3%), that a week-long test after sex can detect whether a person is infected HIV (38.5%), that a woman cannot get HIV if she has anal sex (anal penis penetration) with a man (74.8%), and that a person cannot get HIV if they have oral sex (65.9%). These results indicate that some important information to reduce the incidence of risk behaviors remains poorly understood or unknown among a small proportion of workers despite the higher level of education of this population. This lack of knowledge by most workers contributes to the normalization of HIV/AIDS, both socially and culturally,[13,15] which would exacerbate the stigma and discrimination faced by PLWHAs.[13,16] This would also lead to risky behavior among these workers, who are highly exposed to HIV/AIDS. A study conducted in Kinshasa (in DRC) reported that HIV seropositivity was significantly associated with a poor knowledge level about HIV/AIDS.[9]
In addition, the authors noted that, compared to non-infected individuals, PLWHAs had significant misconceptions related to HIV transmission such that an HIV-infected person cannot appear to be healthy and that HIV is transmitted through witchcraft, God’s punishment, kissing on the mouth, mosquitoes, coughing/sneezing, or undercooked food.[9] In this study, we noted the total score for HIV-KQ-18 (mean of 10.3 out of 18) and the proportion of respondents with a poor knowledge level (81.9%). Again, this finding is surprising when one considers the higher education level of the study population, which is a socio-demographic variable known to influence knowledge, attitudes, and practices regarding HIV/AIDS. However, this lack of knowledge is because, in certain companies or social environments of a certain number of workers, there is little or no mention of the disease. In our view, this lack of knowledge would lead to stigma and discrimination against everything that surrounds the disease. From the point of view of planned behavior theory, this lack of knowledge could be explained by internal non-motivational factors such as the negative social significance given to the disease from its origins,[17] which would explain why some individuals try to stay away from it. It should be recalled that the etiology of HIV/AIDS is prejudiced and perpetuates the idea that the disease is transmitted through deviant or impure sexual practices.[16] Individuals with poor knowledge of the disease can then be expected to experience more external behaviors such as refusal and disdain toward PLWHAs. Misunderstanding of HIV/AIDS can be an important barrier to prevention and education about the disease.[13]
Regarding the determinants of HIV/AIDS knowledge, our results identify that working in a private company (aOR = 2.0 [1.2–3.3]) and having previously tested for HIV/AIDS (aOR = 2.5 [1.5–4.3]) were independently associated with good knowledge level about HIV/AIDS. Voluntary HIV counseling and testing offers benefits that go far beyond diagnosis alone. As our results show, participants who had previously been tested for HIV/AIDS had good knowledge level about HIV/AIDS. It appears that these services contribute to a generalization of lower-risk behaviors and can also act against ignorance, fear and stigma.
The majority of participants had positive attitudes toward PLWHAs and towards various HIV/AIDS situations. For example, most workers agree that PLWHAs have the right to work. In this study, 87.4% of the respondents disagreed that a PLWHA should be excluded from the workplace; almost 8 agreed and almost 5 were not sure. In Tee and Huang’s study,[10] 54.3% of the respondents were comfortable working with a PLWHA, almost one-third (29.5%) were not sure and 16.2% were uncomfortable working with a PLWHA. According to several authors, concerns about the presence of an HIV-infected employee in the workplace included increased medical insurance costs and other additional expenses for the company, as well as the harmony and image of the company in the workplace.[18-20]
Educational programs and interventions should focus not only on improving knowledge about HIV/AIDS but also on reducing negative attitudes towards PLWHAs. Accurate and practical information on different modes of HIV transmission should be disseminated to dispel misconceptions about HIV/ AIDS.[10]
This study has several strengths and limitations that are worth discussing. The response rate in this study (93.8%) suggests that selection bias has been minimized and that our sample is representative. To ensure the quality of our measurements, participants’ knowledge, attitudes, and practices were measured through the cross-cultural adaptation of an existing instrument (HIV-KQ-18) and questions used in the previous studies. One of the strengths of the present study was the use of multivariate models to identify predictors of participants’ level of knowledge, which minimized the potential for confusion bias. The statistical power of our model was also maximized by the substantial size of our sample (n = 563). Finally, since our participants all lived and worked in Lubumbashi, it is important to conduct similar studies in other towns of the DRC to assess the external validity of the study.
CONCLUSION
The present study shows that workers in Lubumbashi have predominantly a poor knowledge level about HIV/AIDS infection despite positive attitudes toward PLWHA and the disease. It leads us to conclude that there is still a high rate of respondents in this professional environment who have incorrect knowledge about HIV/AIDS and its forms of transmission. This suggests that a lack of understanding of HIV/AIDS may have an impact on the risk behaviors of HIV/AIDS among the workers who participated in this study. Thus, our results show the importance of developing prevention campaigns among all workers.
Data availability
The datasheet used to support the findings of this study are available from the corresponding author on request.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- What Drives the HIV/AIDS Epidemic in SubSaharan Africa? Rev Econo Dév. 2009;17:73-106.
- [Google Scholar]
- Stratégie Mondiale du Secteur de la Santé Contre le VIH 2016-2021 Vers L'élimination du Sida. 2016. Genève: OMS; Available from: https://apps.who.int/iris/bitstream/handle/10665/250576/WHO-HIV-2016.05-fre.pdf?sequence=1 [Last accessed on 2022 Feb 21]
- [Google Scholar]
- Fiche D'information 2020 Dernières Statistiques sur L'état de L'épidémie de Sida. Available from: https://www.unaids.org/fr/resources/fact-sheet [Last accessed on 2022 Feb 21]
- [Google Scholar]
- Rapport National de Suivi de la Riposte au VIH/ Sida. 2020. PNMLS: Kinshasa. Available from: https://pnmls.cd/Documentation/uploads/RAPPORT20GAM20202020-20FINAL2018112020.pdf [Last accessed on 2022 Feb 21]
- [Google Scholar]
- Risk perception, HIV/AIDS-related knowledge, attitude and practice of the university community: The case of Ethiopian civil service college. HIV AIDS Rev. 2014;13:26-32.
- [CrossRef] [Google Scholar]
- Knowledge of HIV/AIDS and sexual behavior among the Youths in South West Nigeria, department of guidance and counseling, Uni-versity of Ado-ekiti, Ekiti State, Nigeria. Hum Soc Sci J. 2008;3:81-8.
- [Google Scholar]
- Ministère de la Santé Publique (MSP) et ICF International, 2014 In: Enquête Démographique et de Santé en République Démocratique du Congo 2013-2014 Rockville. Maryland, USA: MPSMRM, MSP et ICF International; 2014.
- [Google Scholar]
- Misconceptions about HIV infection in Kinshasa (Democratic Republic of Congo): A case-control study on knowledge, attitudes and practices. Sex Transm Infect. 2015;91:334-7.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge of HIV/AIDS and attitudes towards people living with HIV among the general staff of a public university in Malaysia. J Soc Aspects HIV AIDS. 2009;6:179-87.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge, attitude and practices of Egyptian industrial and tourist workers towards HIV/AIDS. Eastern Mediterr Health J. 2008;14:1126-35.
- [Google Scholar]
- Development and psychometric evaluation of the Brief HIV Knowledge Questionnaire. AIDS Educ Prev. 2002;14:172-82.
- [CrossRef] [PubMed] [Google Scholar]
- Attitudes et connaissances d'étudiants universitaires à l'égard du VIH-sida. Serv Soc. 2017;63:1-20.
- [CrossRef] [Google Scholar]
- HIV knowledge and associated factors among Internet-using men who have sex with men (MSM) in South Africa and the United States. PLoS One. 2012;7:e32915.
- [CrossRef] [PubMed] [Google Scholar]
- Récits de souffrance et VIH/sida: Réflexions sur quelques enjeux anthropologiques et éthiques du témoignage. Alterstice. 2011;1:97-108.
- [CrossRef] [Google Scholar]
- Représentations sociales du VIH/sida chez les étudiants de niveau universitaire d'une région éloignée du Québec. Can Soc Work Rev. 2015;32:167-86.
- [CrossRef] [Google Scholar]
- When sex equals AIDS: Symbolic stigma and heterosexual adults' inaccurate beliefs about sexual transmission of AIDS. Soc Probl. 2005;52:15-37.
- [CrossRef] [Google Scholar]
- The impact of HIV/ AIDS on small and medium enterprises in South Africa. S Afr J Econ. 2002;70:1217-34.
- [CrossRef] [Google Scholar]
- HIV and the workplace: Organisational consequences of hiring persons with HIV and attitudes towards disclosure of HIV-related information. Int J Manpow. 2000;21:129-40.
- [CrossRef] [Google Scholar]
- Stigma in the workplace: Employer attitudes about people with HIV in Beijing, Hong Kong, and Chicago. Soc Sci Med. 2008;67:1541-9.
- [CrossRef] [PubMed] [Google Scholar]







