Translate this page into:
Factors Associated with Acceptability of Newborn Screening for Sickle Cell Disease in Lubumbashi City, Democratic Republic of the Congo

*Corresponding author: Olivier Mukuku, Maternal and Child Health, Institut Supérieur des Techniques Médicales de Lubumbashi, Lubumbashi, Democratic Republic of the Congo. oliviermukuku@yahoo.fr
-
Received: ,
Accepted: ,
How to cite this article: Katamea T, Mukuku O, Mpoy CW, Mutombo AK, Luboya ON, Wembonyama SO. Factors associated with acceptability of newborn screening for sickle cell disease in Lubumbashi City, Democratic Republic of the Congo. Glob J Med Pharm Biomed Update 2022;17:5.
Abstract
Objective:
Sickle cell disease (SCD) is a major genetic disease that occurs early in childhood and can cause considerable morbidity and even death. Newborn screening (NBS) is one of the effective health services that have lowered the burden of SCD in wealthy countries. Surprisingly, NBS programs are essentially non-existent in subSaharan Africa, where the majority of babies are born with this condition. The objective of this study was to determine the level of acceptability of NBS and the factors influencing it in the population of Lubumbashi city in the Democratic Republic of the Congo.
Material and Methods:
From December 1, 2020, to December 31, 2020, data on sociodemographic characteristics, knowledge, and attitudes related to NBS for SCD were collected from 2032 adults in Lubumbashi city using a semi-structured and pre-tested questionnaire.
Results:
There was a good knowledge of SCD as a hereditary blood disorder (77.7%). NBS’s acceptability rate was 84.5%. Age (P = 0.002), sex (P = 0.025), and religion (p<0.001) were found to be significantly associated with the NBS acceptability.
Conclusion:
According to the findings of this study, NBS is widely accepted in Lubumbashi. The primary challenges to its adoption are likely to be financial and practical rather than social or cultural.
Keywords
Sickle cell disease
Newborn screening
Acceptability
Determinants
Lubumbashi
INTRODUCTION
Sickle cell disease (SCD), also known as sickle cell anemia, is a blood disease linked to an abnormal hemoglobin structure. It is caused by the synthesis of abnormal hemoglobin, which is associated with a mutation in the gene coding for the production of the β-globin chain and transmitted by both the father and the mother (autosomal recessive disease).[1] As a result, abnormal hemoglobin S is produced (HbS), which causes red blood cell deformation as well as vascular blockage. Sickle cell red blood cells have deformability that is reduced in a way that varies with the genotype and, in the same patient, according to clinical and physiological conditions.[1]
The lack of reliable data in most countries makes it difficult to estimate the number of people affected worldwide. There are no national disease registries, including in developed countries that have had newborn screening (NBS) programs in place for several years (USA, England, and France).[2] Various estimates have been published[2-4] reporting widely varying S-allele distribution frequencies across regions: Sub-Saharan Africa (about 20 countries with 2–38%), India (six regions with 17–30%), Saudi Arabia (1–29%), and Iraq (0–22%). In the Democratic Republic of the Congo (DRC), the latest studies report a prevalence of up to 40% of the population for sickle cell trait (HbS) and up to 2.3% of the population for homozygous form (HbSS). The DRC annually records approximately 40,000 births of children with SCD.[5,6] These births result in early and high mortality. Indeed, 50– 90% of these children die before the age of 5 years. This high mortality rate can be partly explained by the disease’s late diagnosis, a lack of appropriate treatment, and families’ limited resources.[7,8]
SCD is responsible for significant infant mortality in developing countries, where there are no systematic NBS and comprehensive management programs. NBS has been proven to significantly reduce SCD-related mortality in newborns. However, the achievement of this NBS is associated with the notion of its acceptability to the target population, and this acceptability is dependent on several socio-cultural factors which present from one community to another.[9,10]
Causes of SCD differ between and within communities. The traditional therapists seek to link the disease to an organic dysfunction, but most of the population’s attitudes come from the ontological meaning of the disease. Is it a natural disease, a witch attack, an evil sent by ancestors, or by a bush genius? The idea of self-awareness drives the search for remedies and social attitudes. In Central Africa (Congo, DRC, Cameroon, Gabon), the population attributes more diseases, especially chronic ones such as SCD, to the aggression of a sorcerer or the malice or curse of ancestral spirits. It also happens that the patient himself is considered an evil spirit. The search for remedies, apart from medical care, will, then, turn to the countersorcerer or the exorcist.[10,11]
In developing countries, screening for the disease is not systematic and is usually carried out after a first crisis, which can delay the outcome by several months since the primary priority is to treat severe anemia and the complications of the crisis for which the child has been referred.[12] In sub-Saharan Africa, a few pilot projects for routine NBS have been carried out in recent years in Ghana, Uganda, Benin, and the DRC, with external funding, but none, to the best of our knowledge, has succeeded in establishing a national routine NBS program.[6,13-16] Unfortunately, these pilot projects have faced problems such as the NBS acceptability, both among some parents, caregivers, and even the authorities of countries for whom this screening would be an additional burden.[17,18] It is in this context that it is considered that before any implementation of a public health program or project, the bottom-up approach is recommended as it promotes participation and community ownership.[19] With this in mind, and with a view to the future establishment of a systematic national NBS program in the DRC, we proposed to conduct a survey of the NBS acceptability to the population in our area.
The objective of this study is to determine the acceptability level of NBS and to identify factors influencing it in the population in Lubumbashi city, DRC.
MATERIAL AND METHODS
The present study was conducted in Lubumbashi city. Lubumbashi is the capital of the Haut-Katanga Province, located in the Southeast of the DRC. We conducted an analytical cross-sectional study based on a community survey of adults. The survey took place over a period from December 1, 2020, to December 31, 2020. All participants gave their consent to the data collection. A total of 2450 questionnaires were distributed due to 350 per municipality (Lubumbashi city comprises seven municipalities). Of the 2450 adults invited to complete the questionnaire, 2032 agreed to complete the questionnaire and were included in this study. This represented an effective response rate of 82.9%.
The data collection tool of this study is a semi-structured questionnaire used in the previous studies[20,21] that established the validity of the questionnaire content. This questionnaire was developed to obtain information from respondents on sociodemographic factors, NBS knowledge, attitudes about SCD screening policies, and attitudes on voluntary termination of affected pregnancy if the participant is expected to give birth to a child affected by SCD. Answer options for closed questions were “Yes,” “No,” or “Don’t know.”
Three teams, each consisting of six investigators and one physician, were formed to collect data based on a multiple-choice questionnaire in French and Swahili (local language). The survey sheet was either completed by the investigator if the person could not read or write, or completed by the respondent after clarification by the principal investigator. A pilot survey with ten randomly selected subjects was done to see if questionnaire items were simple to grasp. Pilot interviews guaranteed that no unclear questions were given and assessed how long it would take to finish an interview. The interviews lasted about 25 min each. The data from the pilot interviews were not included in the study’s final results. The team had 3 days of training before and after the pre-test. The study concentrated on maintenance practices, the study’s objective, and ethical considerations. Throughout the data collecting period, the lead investigator and supervisors observed the site daily and verified each questionnaire daily to ensure completeness and uniformity.
The collected data were entered into Microsoft Excel 2019 and were checked for inconsistencies and errors. The analyses were performed using STATA software (version 15). Frequencies and means were determined for the sociodemographic characteristics of the participants. The distribution of each item of knowledge (e.g., causality, in utero diagnosis, postnatal, and any other time diagnostic) and attitudes about SCD screening (including pre-marriage, pregnancy, postnatal, and reasons for each decision) were presented in frequency figures and then cross-referenced to sociodemographic variables in a bivariate analysis followed by multivariate analysis. Pearson’s Chi-square test and the adjusted odds ratio (AOR) and 95% confidence interval were calculated to determine the association. p<0.05 was considered statistically significant.
This study was accepted by the University of Lubumbashi’s Medical Ethics Committee (Approval No: UNILU/ CEM/030/2021). The municipal authorities of each municipality surveyed gave the community’s approval. All individuals provided formal permission to participate. An initial explanation of the study’s goal and approach was given to all respondents before conducting the interviews. Participants were reassured that the information they supplied would be kept confidential, that their participation was fully optional, and that they may opt-out or stop participating at any time. Respondents were requested to sign an informed consent declaration.
RESULTS
Out of a total of 2450 respondents, 2032 had agreed to voluntarily respond to our questionnaire, a response rate of 82.9%.
As described in [Table 1], the mean age of respondents was 31.0 ± 9.0 years and 45.23% (919/2032) were between 21 and 30 years of age; 53.89% were female and 46.11% were male. Regarding marital status, 1103 (54.28%) of respondents reported being single, 805 (39.62%) were married, and 124 (6.10%) were separated/divorced. In terms of occupation, 806 (39.67%) reported doing business, 499 (24.56%) were employed, 426 (20.96%) had no occupation (unemployed), and 301 (14.81%) did other activities than business. As for religion, 856 (42.13%) were Pentecostal/Protestant, 816 (40.16%) were Catholic, 137 (6.74%) were Muslim, and 223 (10.97%) were reported belonging to other religious groups. Almost 40% of the respondents had a higher/ university level, 43.75% had a secondary level, 13.24% had a primary level, and 3.54% were illiterate.
| Variable | Number (n=2032) | Percentage |
|---|---|---|
| Age (years) | ||
| <21 | 199 | 9.79 |
| 21–30 | 919 | 45.23 |
| 31–40 | 694 | 34.15 |
| ≥41 | 220 | 10.83 |
| Mean±standard deviation | 31.0±9.0 | |
| Sex | ||
| Female | 1095 | 53.89 |
| Male | 937 | 46.11 |
| Marital status | ||
| Single | 1103 | 54.28 |
| Married | 805 | 39.62 |
| Separate/divorced | 124 | 6.10 |
| Educational level | ||
| Illiterate | 72 | 3.54 |
| Primary | 269 | 13.24 |
| Secondary | 889 | 43.75 |
| Higher/university | 802 | 39.47 |
| Occupation | ||
| Business | 806 | 39.67 |
| Employed | 499 | 24.56 |
| Unemployed | 426 | 20.96 |
| Others | 301 | 14.81 |
| Religion | ||
| Pentecostal/Protestant | 856 | 42.13 |
| Catholic | 816 | 40.16 |
| Muslim | 137 | 6.74 |
| Other religious groups | 223 | 10.97 |
Knowledge of SCD as a hereditary blood disorder was good (77.71%), 1545 (76.03%) knew that SCD is inherited from both parents, and 1516 (74.61%) knew that it was not contagious [Figure 1]. Regarding beliefs about SCD, 1055 (51.92%) said that it is God’s will, 389 (19.14%) said that it is God’s punishment, and 320 (15.75%) thought that it is the work of the devil or evil spirits.
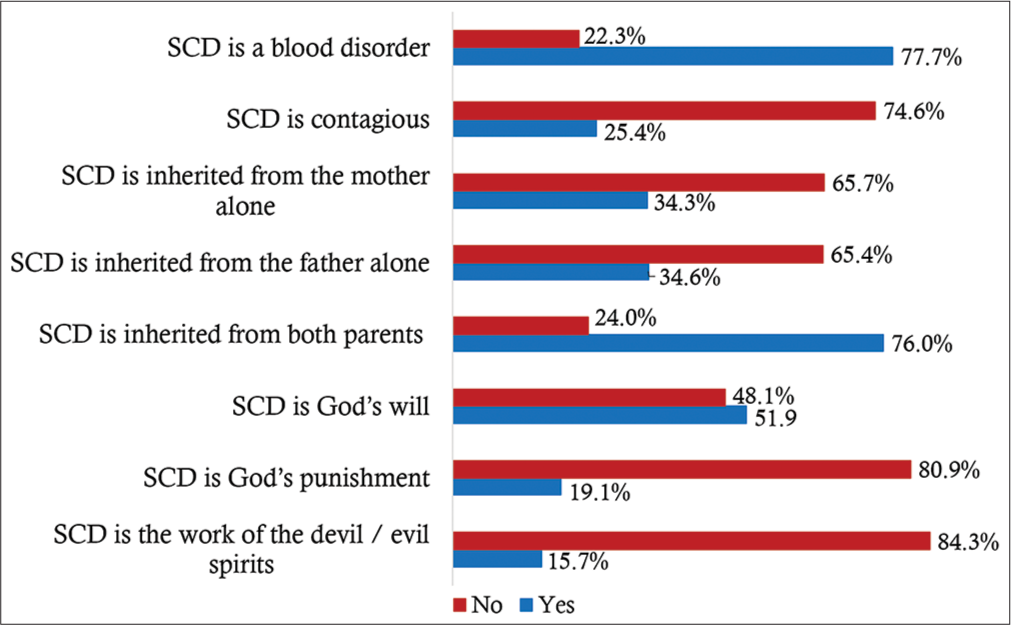
- Knowledge of sickle cell disease among 2032 survey respondents.
Three hundred and seventy-seven respondents (18.55%) were aware of their sickle cell status and 20 (5.31%) indicated that they were homozygous sickle cell patients (Hb SS) and 54 (14.32%) had a sickle cell trait (Hb AS).
As shown in [Figure 2], 1584 (77.95%) respondents reported that SCD can be diagnosed at any time in a person’s life, 1043 (51.33%) knew that it can be diagnosed at birth (neonatal diagnosis), and 914 (44.98%) said that it can be diagnosed before birth (prenatal diagnosis).
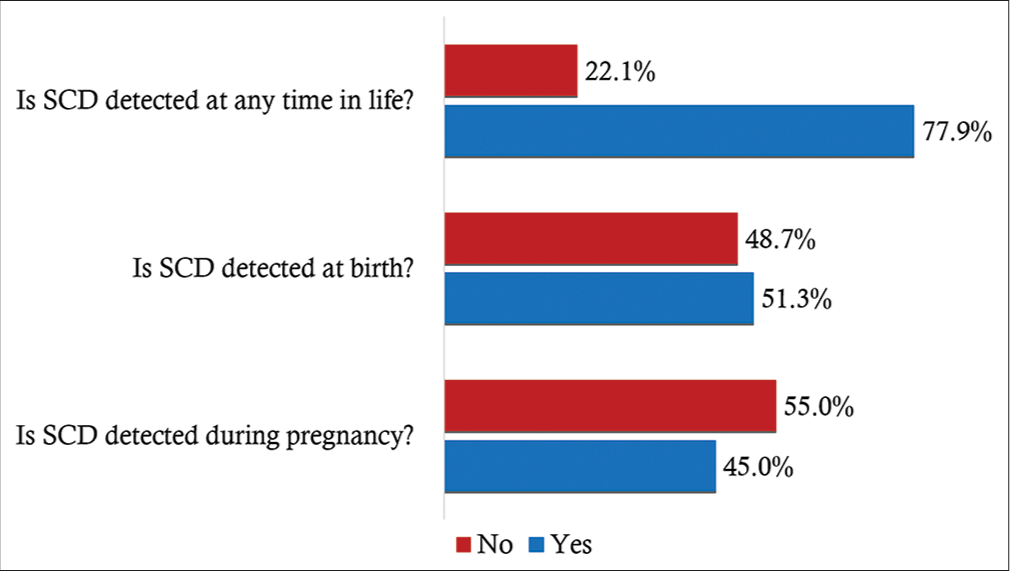
- Knowledge of SCD screening period among 2032 survey respondents.
In terms of respondents’ attitudes toward SCD screening, the most acceptable form of SCD screening was premarital (88.98%), while the least acceptable was neonatal (84.50%). SCD screening of family members and all pregnant women was also acceptable for 87.60% and 86.17%, respectively [Figure 3].

- Attitudes toward SCD screening among 2032 survey respondents.
We examined responses from respondents regarding the termination of a pregnancy with a fetus with SCD. Almost nine in 10 respondents (1780/2032; 87.60%) were against terminating the pregnancy and 12.40% (252/2,032) were in favor of terminating the pregnancy. The most advanced reasons for opposing the termination of the pregnancy were religious (65.71%) followed by ethical considerations (34.29%). On the other hand, for reasons given by respondents who were in favor of terminating the pregnancy, we noted that social considerations came first (49.56%) followed by economic considerations (32.46%).
[Table 2] shows relationships between the NBS acceptability and sociodemographic characteristics of the respondents. We found that age, sex, and religion were significantly associated with the NBS acceptability (P < 0.05). However, no significant relationship was noted between the NBS acceptability and the following variables: Marital status, educational level, and occupation.
| Variable | Total=2032 | Respondents accepting the NBS=1717 n (%) | χ2 | P-value |
|---|---|---|---|---|
| Age (years) | 14.37 | 0.002 | ||
| <21 | 199 | 150 (75.38) | ||
| 21–30 | 919 | 790 (85.96) | ||
| 31–40 | 694 | 589 (84.87) | ||
| ≥41 | 220 | 188 (85.45) | ||
| Sex | 5.03 | 0.025 | ||
| Male | 937 | 773 (82.50) | ||
| Female | 1095 | 944 (86.21) | ||
| Marital status | 2.58 | 0.275 | ||
| Single | 1103 | 921 (83.50) | ||
| Married | 805 | 693 (86.09) | ||
| Separate/divorced | 124 | 103 (83.06) | ||
| Educational level | 2.14 | 0.343 | ||
| Illiterate/primary | 341 | 284 (83.28) | ||
| Secondary | 889 | 763 (85.83) | ||
| Higher/university | 802 | 670 (83.54) | ||
| Religion | 95.29 | <0.001 | ||
| Pentecostal/Protestant | 856 | 723 (84.46) | ||
| Catholic | 816 | 723 (88.60) | ||
| Muslim | 137 | 77 (56.20) | ||
| Other religious groups | 223 | 194 (87.00) | ||
| Occupation | 6.88 | 0.075 | ||
| Unemployed | 426 | 356 (83.57) | ||
| Business | 806 | 665 (82.51) | ||
| Employed | 499 | 437 (87.58) | ||
| Other activities | 301 | 259 (86.04) |
Proportions of NBS acceptability were 75.38%, 85.96%, 84.87%, and 85.45%, respectively, among respondents <21 years, 21–30 years, 31–40 years, and ≥41 years of age. The comparison between these rates was statistically significant (χ2 = 14.37; P = 0.002). Respondents ≥21 years of age were more likely to accept the NBS than those <21 years of age [Table 3].
| Variable | Adjusted odds ratio | Standard error | t-value | P-value | 95% confidence interval | Sig. | |
|---|---|---|---|---|---|---|---|
| Age (years) | |||||||
| <21 | 1.00 | - | - | - | - | - | |
| 21–30 | 1.95 | 0.38 | 3.36 | 0.001 | (1.32 | 2.87) | *** |
| 31–40 | 1.84 | 0.39 | 2.86 | 0.004 | (1.21 | 2.79) | *** |
| ≥41 | 1.74 | 0.49 | 1.97 | 0.049 | (1.00 | 3.02) | ** |
| Sex | |||||||
| Male | 1.00 | - | - | - | - | - | |
| Female | 1.31 | 0.18 | 1.98 | 0.048 | (1.00 | 1.72) | ** |
| Marital status | |||||||
| Single | 1.00 | - | - | - | - | - | |
| Married | 1.34 | 0.21 | 1.92 | 0.055 | (0.99 | 1.81) | * |
| Separate/Divorced | 1.15 | 0.32 | 0.49 | 0.625 | (0.67 | 1.97) | * |
| Educational level | |||||||
| Illiterate/primary | 1.00 | - | - | - | - | - | |
| Secondary | 1.03 | 0.19 | 0.15 | 0.881 | (0.71 | 1.49) | * |
| Higher/university | 0.87 | 0.16 | -0.78 | 0.435 | (0.60 | 1.25) | * |
| Religion | |||||||
| Pentecostal/Protestant | 1.00 | - | - | - | - | - | |
| Catholic | 1.50 | 0.23 | 2.61 | 0.009 | (1.11 | 2.02) | *** |
| Muslim | 0.24 | 0.05 | −7.01 | <0.001 | (0.16 | 0.36) | *** |
| Other religious groups | 1.25 | 0.28 | 0.98 | 0.326 | (0.80 | 1.95) | * |
| Occupation | |||||||
| Unemployed | 1.00 | - | - | - | - | - | |
| Business | 1.04 | 0.19 | 0.24 | 0.812 | (0.74 | 1.48) | * |
| Employed | 1.48 | 0.30 | 1.91 | 0.056 | (0.99 | 2.20) | * |
| Other activities | 1.50 | 0.35 | 1.72 | 0.085 | (0.95 | 2.38) | * |
Proportions of NBS acceptability were statistically higher in female respondents (86.21%) than in male respondents (82.50%) (χ2 = 5.03; P = 0.025). We found that women accepted the NBS more than men (aOR = 1.31 [1.00–1.72]; P = 0.048).
Proportions of NBS acceptability were 88.60%, 87.00%, 56.20%, and 84.46%, respectively, among Catholics, Protestants/Pentecostals, Muslims, and other religious groups. Pearson test shows a statistically significant difference between these rates (χ2 = 95.29; P < 0.001). Compared to Protestants/Pentecostals, Catholics were more likely to accept the NBS (aOR = 1.50 [1.11–2.02]; P = 0.009); Muslims, on the other hand, were less accepting the NBS (aOR=0.24 [0.16–0.36]); P < 0.001).
DISCUSSION
The acceptability of the SCD NBS is a relatively unstudied area. To the best of our knowledge, this study is the first in Lubumbashi, and one of the few in the DRC and sub-Saharan Africa assessing the population’s knowledge and attitudes toward the NBS. The main public health message of this study is the good acceptability of NBS (84.50%) in our population. Such a prevalence is indicative of support for a systematic NBS program. This acceptability rate is relatively close to 86% noted by Oluwole et al.[22] and 86.1% found by Nnodu et al.[21] in Nigeria. Higher rates have been reported: 99% by Tubman et al.[23] in Liberia and 99.7% by Odunvbun et al.[24] in Nigeria. Contrary to our results, a recent study conducted in Koula-Moutou (Gabon) found a low acceptability rate of 30%.[25]
The present study shows that there are several misconceptions about SCD among the respondents, although the level of knowledge was good. Supernatural explanations of the cause of SCD are common in many settings in Africa.[26] Given that the NBS is based on public trust and opinion, these misbeliefs must be adequately addressed not only at all levels of health care but also through functional cross-sectoral collaboration, particularly with the media.[21]
Only 18.5% of respondents knew their sickle cell status. Although higher than those reported in Nigeria (3.5%),[21] our results show a lack of SCD screening in the Congolese population. Increased awareness and knowledge of SCD status have been identified as important to strengthen public health efforts to control SCD, particularly in high prevalence settings.[27]
One of the main objectives of this study was to determine the factors to be considered in encouraging participation in NBS programs, which would maximize the cost-effectiveness of the program once implemented. Our results show that the level of acceptability of the NBS was independently associated with age and gender. Unlike the Nnodu et al.,[21] this study notes that younger respondents (<21 years) were less favorable to the NBS.
The present study shows that female respondents were more likely to accept the NBS than male respondents. We believe that the fact that women are the majority caregivers in our African societies means that they become more sensitive to children’s health problems than men and readily accept NBS.
As in the Nigerian study,[21] the present study shows that religion was one of the variables independently associated with the acceptability of the NBS. Our results show that, compared to Protestants/Pentecostals, Catholics were more likely to accept the NBS; Muslims, however, were less accepting of the NBS. This finding is consistent with that made by Nnodu et al.[21] who found that Muslims were less favorable to the NBS. Our results are partly explained by the fact that a large majority of Christian churches require couples intending to be married to be screened for SCD before marriage. There is, therefore, a need to increase mass mobilization and awareness efforts with appeals to religious leaders to show interest in premarital SCD counseling and testing.
In developed countries, NBS, when paired with adequate follow-up and care for SCD children in specialized clinics, reduced the SCD death rate from 16% to <1%.[28,29] It is acknowledged in developing countries that an unknown percentage of children with SCD are likely to die as a result of the condition remaining undetected, untreated, or undertreated.[30] Since the provision of services in the DRC is hampered by major economic and organizational difficulties, the results of this study are an invitation to health authorities to implement a national NBS policy so that children with SCD can benefit from medical care and monitoring throughout their lives.
As for the strengths of the present study, we recall that this is the first study to address the issue of the NBS acceptability in the DRC. Its results are answers to the many questions raised by various systematic NBS projects carried out in the DRC. Its large sample (n=2032) contributed to statically significant associations between NBS acceptability and factors that appear to influence it. These associations are very useful because they provide both the directions of public awareness policies regarding NBS and an understanding of independent factors influencing it. A major limitation of this study is that it would have the possibility of selection bias because our study population is only urban. Thus, the results of that study could be considered applicable only to the urbanized population. Despite this limitation, the results of the current research are an acceptable starting point for initiating a discussion on a national policy for the NBS.
CONCLUSION
This study has shown that NBS is acceptable to the population in Lubumbashi city. This is encouraging given the establishment of a systematic NBS program to reduce the burden of SCD in the DRC. However, the present study reveals and highlights the need for public education to move away from the misconceptions about SCD and increase acceptance in all sectors of the community. As a result, there is a growing interest in training genetic counselors and incorporating genetic services into primary care, given that genetic diseases are becoming a significant public health problem.
Data availability
The datasheet used to support the findings of this study is available from the corresponding author on request.
Declaration of the patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Physiopathologie de la drépanocytose In: de Montalembert, Allali S, Brousse V, Marchetti MT, eds. La Drépanocytose de L'enfant et L'adolescent. Paris: Elsevier Masson; 2020.
- [CrossRef] [PubMed] [Google Scholar]
- Global epidemiology of sickle haemoglobin in neonates: A contemporary geostatistical model-based map and population estimates. Lancet. 2013;381:142-51.
- [CrossRef] [Google Scholar]
- Global epidemiology of haemoglobin disorders and derived service indicators. Bull WHO. 2008;86:480-7.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of haemoglobin disorders in Europe: An overview. Scand J Clin Lab Invest. 2007;67:39-69.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal screening and clinical care programs for sickle cell disorders in Sub-Saharan Africa: Lessons from pilot studies. Public Health. 2008;122:933-41.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal screening for sickle cell anaemia in the democratic Republic of the Congo: experience from a pioneer project on 31 204 newborns. Transfus Med. 2010;20:62-5.
- [CrossRef] [PubMed] [Google Scholar]
- Sickle cell disease in Africa: A neglected cause of early childhood mortality. Am J Prev Med. 2011;41(6 Suppl 4):S398-405.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of a density-based rapid diagnostic test for sickle cell disease in a clinical setting in Zambia. PLoS One. 2014;9:e114540.
- [CrossRef] [PubMed] [Google Scholar]
- Perceptions of young adults with sickle cell disease concerning their disease experience. J Adv Nurs. 2016;72:1441-51.
- [CrossRef] [PubMed] [Google Scholar]
- Optimism and perceived stress in sickle-cell disease: The role of an afrocultural social ethos. J Black Psychol. 2011;37:234-53.
- [CrossRef] [Google Scholar]
- Perceptions and practice of early diagnosis of sickle cell disease by parents and physicians in a Southwestern state of Nigeria. Sci World J. 2020;2020:4801087.
- [CrossRef] [PubMed] [Google Scholar]
- Newborn screening for sickle cell disease and other hemoglobinopathies. J Am Med Assoc. 1987;258:1205-9.
- [CrossRef] [Google Scholar]
- Screening newborns for sickle cell disease in Ghana. Pediatrics. 2008;12:5-7.
- [CrossRef] [Google Scholar]
- Sickle cell disease screening in Northern Nigeria: The CoExistence of B-thalassemia inheritance. Pediatr Ther. 2015;5:262.
- [CrossRef] [Google Scholar]
- Newborn screening for sickle cell disease in Republic of Benin. J Clin Pathol. 2009;62:46-8.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of sickle cell trait and disease in the Uganda sickle surveillance study (US3): A cross-sectional study. Lancet Glob Health. 2016;4:e195-200.
- [CrossRef] [Google Scholar]
- Newborn screening for sickle cell disease in Lubumbashi, DRC. Rev Inf Congolais. 2018;2:62-3.
- [Google Scholar]
- Newborn screening for sickle cell disease in Lubumbashi city, Democratic Republic of Congo: A preliminary study on an update of the disease prevalence. Br J Haematol. 2021;193(Suppl 1):31.
- [Google Scholar]
- Acceptability of childhood screening: A systematic narrative review. Public Health. 2021;193:126-38.
- [CrossRef] [PubMed] [Google Scholar]
- Acceptability of prenatal diagnosis by a sample of parents of sickle cell anemia patients in Cameroon (SubSaharan Africa) J Genet Couns. 2011;20:476-85.
- [CrossRef] [PubMed] [Google Scholar]
- A multi-centre survey of acceptability of newborn screening for sickle cell disease in Nigeria. Cureus. 2018;10:e2354.
- [CrossRef] [PubMed] [Google Scholar]
- Feasibility and acceptability of early infant screening for sickle cell disease in Lagos, Nigeria a pilot study. PLoS One. 2020;15:e0242861.
- [CrossRef] [PubMed] [Google Scholar]
- Newborn screening for sickle cell disease in Liberia: A pilot study. Pediatr Blood Cancer. 2016;63:671-6.
- [CrossRef] [PubMed] [Google Scholar]
- Newborn screening for sickle cell disease in a Nigerian hospital. Public Health. 2008;122:1111-6.
- [CrossRef] [PubMed] [Google Scholar]
- Acceptability of neonatal sickle cell disease screening among parturient women at the Paul Moukambi Regional Hospital in rural Eastern Gabon, Central Africa. Afr J Reprod Health. 2021;25:72-7.
- [Google Scholar]
- "All her children are born that way": Gendered experiences of stigma in families affected by sickle cell disorder in rural Kenya. Ethn Health. 2011;16:343-59.
- [CrossRef] [PubMed] [Google Scholar]
- Sickle cell disease: The need for a public health agenda. Am J Prev Med. 2011;41:S376-83.
- [CrossRef] [PubMed] [Google Scholar]
- Malaria as a cause of morbidity and mortality in children with homozygous sickle cell disease on the coast of Kenya. Clin Infect Dis. 2009;49:216-22.
- [CrossRef] [PubMed] [Google Scholar]
- Implementation of universal newborn bloodspot screening for sickle cell disease and other clinically significant haemoglobinopathies in England: Screening results for 2005-7. J Clin Pathol. 2009;62:26-30.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality in sickle cell anemia in Africa: A prospective cohort study in Tanzania. PLoS One. 2011;6:e14699.
- [CrossRef] [PubMed] [Google Scholar]







