Translate this page into:
A Pragmatic Classification of Motor Abnormalities Seen in Clinical Psychiatric Practice

*Corresponding author: Dr. Jagdish Varma, Department of Psychiatry, Pramukhswami Medical College, Karamsad, Gujarat, India. jagdishrv@charutarhealth.org
-
Received: ,
Accepted: ,
How to cite this article: Dharaiya D, Varma J. A Pragmatic Classification of Motor Abnormalities Seen in Clinical Psychiatric Practice. Glob J Med Pharm Biomed Update. 2024;19:15. doi: 10.25259/GJMPBU_4_2024
Abstract
This manuscript presents a pragmatic classification of motor abnormalities commonly observed in psychiatric practice. The classification is divided into quantitative and qualitative categories, with a focus on motor underactivity and overactivity. The quantitative category includes symptoms such as retardation, hyperactivity, obsessive slowness, and agitation. The qualitative category explores catatonic symptoms, including motoric immobility, extreme agitation, extreme negativism, posturing, and echo phenomenon. In addition, non-catatonic/neurological motor abnormalities are discussed, such as hypokinetic and hyperkinetic symptoms. The manuscript also highlights related concepts, including La-belle indifference. This classification provides a valuable framework for understanding and diagnosing motor abnormalities in psychiatric practice.
Keywords
Movement disorder
Motor disorder
Classification
INTRODUCTION
Motor abnormalities are commonly observed in psychiatric practice and can provide valuable insights into the underlying conditions.[1] This article presents a pragmatic classification of motor abnormalities, categorizing them into quantitative and qualitative abnormalities [Figure 1].[2]
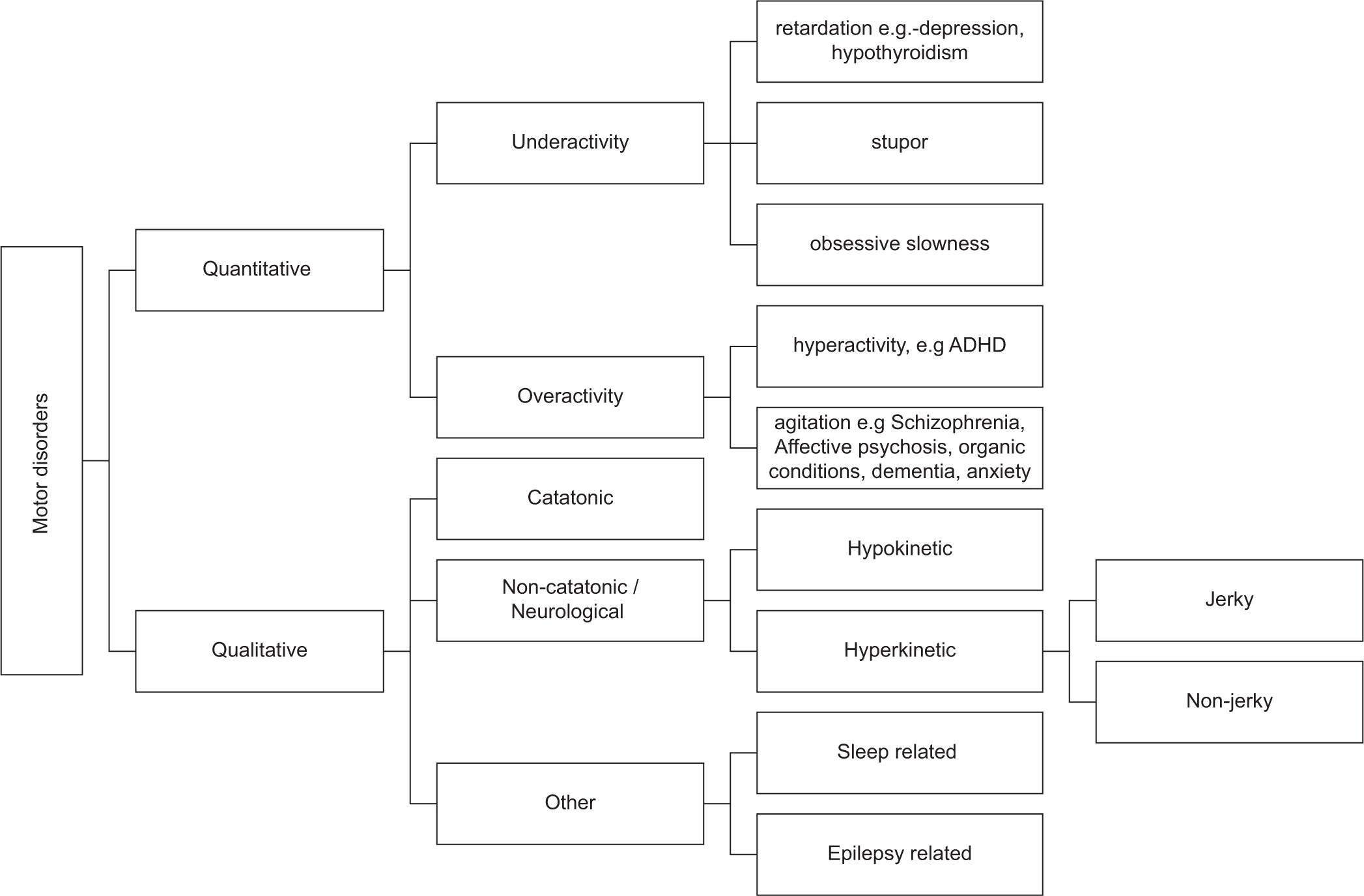
- General scheme for classification of motor disorders.
The classification aims to provide a broad framework for understanding and identifying these abnormalities in clinical practice and an aide-memoir for the trainee.
DISCUSSION
Quantitative abnormalities
Quantitative abnormalities refer to variations in the level of motor activity. They can be further classified into underactivity and overactivity. Underactivity includes retardation, obsessive slowness, and stupor. Retardation refers to slowness in the initiation, execution, and completion of actions. Obsessive slowness is characterized by slowness secondary to repeated doubts and compulsive rituals. Stupor is a state of markedly slowed motor activity, often to the point of immobility and seeming unawareness of surroundings.
Overactivity includes hyperactivity and agitation. Hyperactivity is characterized by increased motor activity numerous and quick movements and gestures, but with a specific purpose. Agitation refers to excessive motor activity and restlessness without a specific purpose. It may manifest as drumming the fingers, rubbing the hands, getting up and sitting down nonstop, or scratching the head.
Qualitative abnormalities
Qualitative abnormalities involve specific patterns of motor behavior and can be further categorized into catatonic, noncatatonic, and other abnormalities. Catatonic abnormalities are characterized by a range of motor symptoms and can be assessed using the Diagnostic and Statistical Manual (DSM) criteria.[3] DSM-5 notes 12 symptoms out of which three are required for diagnosis. The MEEPE mnemonic may be used to remember the symptoms [Supplementary Table 1].[3] However, there are several other symptoms of catatonia which can be named non-DSM symptoms. These non-DSM symptoms are described according to the Bush-Francis scale [Supplementary Table 2].[4]
Apart from catatonic abnormalities, there are other motor abnormalities that can be observed in psychiatric practice. These abnormalities have a neurological basis and can be classified into hypokinetic and hyperkinetic categories [Figure 2].[5] Hypokinetic abnormalities are characterized by reduced movement and include symptoms such as bradykinesia, rigidity, postural instability (seen in parkinsonism), and apraxia [Supplementary Table 3].[5]
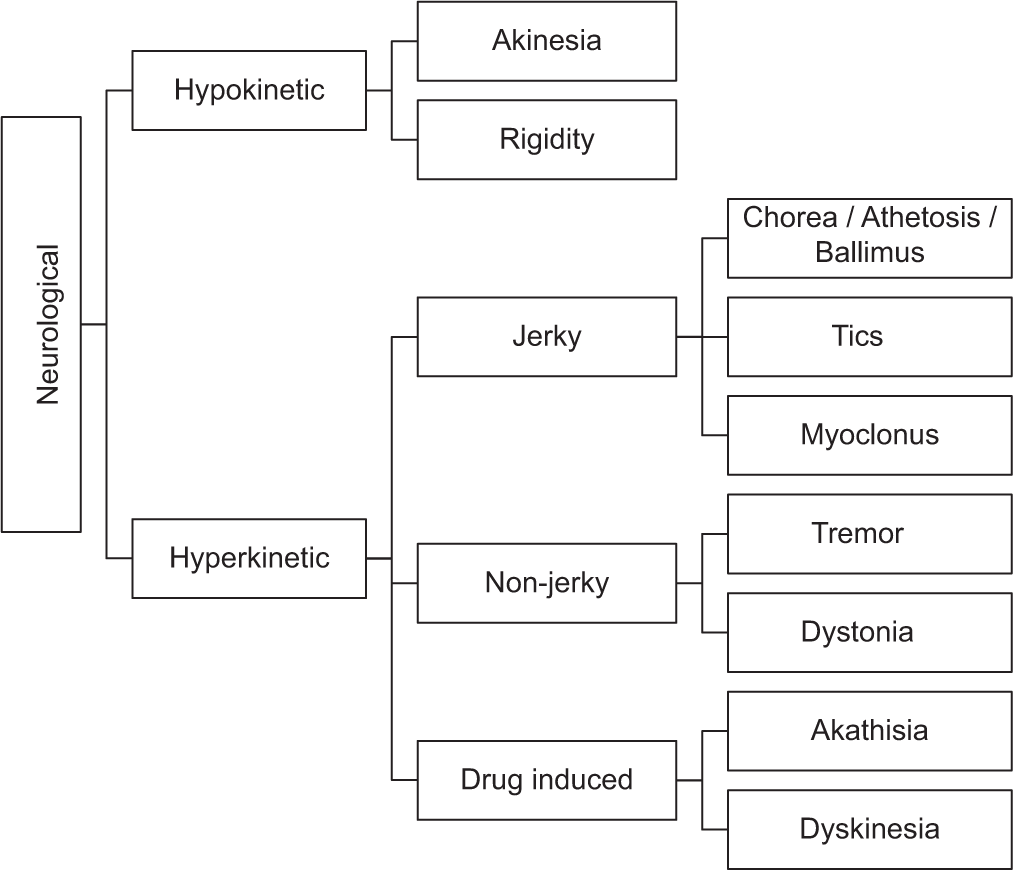
- Classification of non-catatonic/neurological motor abnormalities.
Hyperkinetic abnormalities involve excessive and abnormal movements and are further clinically differentiated as jerky or non-jerky.[6] Hyperkinetic abnormalities include symptoms such as tremors, chorea/athetosis/ballismus, tics, dystonia, myoclonus, akathisia, dyskinesia, and ataxia [Supplementary Table 4].[5,7]
In addition to the above categories, there are motor abnormalities that are related to sleep disorders and epilepsy. Sleep-related motor abnormalities can manifest as dyssomnias or parasomnias [Supplementary Table 5].[8,9] Dyssomnias are a broad category of sleep disorders that involve difficulties with falling asleep, staying asleep, or excessive sleepiness. Parasomnias are a category of sleep disorders that involve abnormal behaviors, movements, emotions, perceptions, or dreams that occur during sleep or the transition between wakefulness and sleep. Whereas motor abnormalities are not pathognomonic of epilepsy, several motor symptoms can be associated with epilepsy. Depending on the specific seizure type, these abnormalities can present as various types of motor movements [Supplementary Table 6].[10-12] Astasia-abasia is an inability to stand or walk normally, even though normal leg movements can be performed in a sitting or lying down position. The gait is bizarre and does not suggest a specific organic lesion as seen in conversion disorder. La-belle indifference refers to a lack of psychological distress or concern about physical symptoms or disabilities, even when they are significant.
CONCLUSION
It is important to note that the classification presented here provides a broad framework for understanding motor abnormalities in psychiatric practice. There may be some overlap between the quantitative and qualitative categories, and certain symptoms can be classified into multiple categories. In addition, abnormal facial expressions and abnormal eye movements are considered part of the description of appearance. The purpose of this classification is to provide a useful tool for beginners in the field and to facilitate the identification and understanding of motor abnormalities in clinical practice.
This article presents a pragmatic classification of motor abnormalities seen in psychiatric practice, which can serve as a valuable tool for clinicians in understanding and identifying motor abnormities in their clinical practice.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Fundamentals of Psychiatry for Health Care Professionals Berlin: Springer; 2022.
- [CrossRef] [Google Scholar]
- Diagnostic and Statistical Manual of Mental Disorders (5th ed). United States: American Psychiatric Association; 2013.
- [CrossRef] [Google Scholar]
- Catatonia. I. Rating Scale and Standardized Examination. Acta Psychiatr Scand. 1996;93:129-36.
- [CrossRef] [PubMed] [Google Scholar]
- A Practical Approach to Movement Disorders: Diagnosis and Management Berlin: Springer Publishing Company; 2021.
- [CrossRef] [Google Scholar]
- The Clinical Approach to Movement Disorders. Nat Rev Neurol. 2010;6:29-37.
- [CrossRef] [PubMed] [Google Scholar]
- Movement Disorders: A Brief Practical Approach to Diagnosis and Management. J R Coll Physicians Edinb. 2006;36:331.
- [Google Scholar]
- The International Classification of Sleep Disorders (ICSD-3) United States: American Academy of Sleep Medicine; 2014.
- [Google Scholar]
- Descriptive Psychopathology: The Signs and Symptoms of Behavioral Disorders United Kingdom: Cambridge University Press; 2008.
- [CrossRef] [Google Scholar]
- The Neuropsychiatry of Epilepsy (2nd ed). United Kingdom: Cambridge University Press; 2011.
- [CrossRef] [Google Scholar]
- Oxford Textbook of Epilepsy and Epileptic Seizures Oxford: OUP Oxford; 2012.
- [CrossRef] [Google Scholar]
- Frontal Lobe Seizures: Overview and Update. J Neurol. 2022;269:3363-71.
- [CrossRef] [PubMed] [Google Scholar]







