Translate this page into:
Vitamin D Status and its Association with Lipid Profile among Medical Undergraduates in a Medical College in Kerala

*Corresponding author: K. Annapurna, Department of Physiology, Government Medical College, Kannur, Kerala, India. dr.annapurnak@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Annapurna K, Swarnalatha PK. Vitamin D Status and its Association with Lipid Profile among Medical Undergraduates in a Medical College in Kerala. Glob J Med Pharm Biomed Update 2020;15:7.
Abstract
Objectives:
To assess the vitamin D status among the study population and to determine the association between Vitamin D deficiency and dyslipidemia.
Materials and Methods:
This cross sectional study included medical undergraduates aged between 18-20 years with no major illness or medication history. Complete fasting lipid profile was measured by photometry method and biochemical estimation of serum 25-hydroxy 25(OH)D was done using automated chemiluminescent immunoassay. Vitamin D status and lipid profile parameters were compared using Pearson Chi-square test. P < 0.05 was considered as statistically significant. Descriptive statistics such as mean, standard deviation, and inferential statistics like Chi-square test were used.
Results:
96.6% were vitamin D deficient and 40% of the subjects were dyslipidemic. There was no significant association between Vitamin D status and Lipid profile.
Conclusion:
High prevalence of Vitamin D deficiency but no significant association between vitamin D deficiency and dyslipidemia.
Keywords
Vitamin D
Deficiency
Dyslipdemia
Medical undergraduates
INTRODUCTION
Vitamin D, also known as the sun-shine vitamin, is synthesized in the skin, by direct absorption of ultraviolet B radiation. It can also be obtained through Vitamin D fortified foods and oral supplements, but is present naturally in only very few food items such as oily fish, certain types of mushrooms, and egg yolk.
In the liver, Vitamin D is hydroxylated to form 25-hydroxyvitamin D (25(OH)D). The serum level of 25(OH)D is the standard criterion for determining whole-body Vitamin D status.
At present, Vitamin D status is categorized by endocrine society guidelines as deficiency, insufficiency, and sufficiency based on serum 25(OH)D levels below 20 ng/ml, 21–29 ng/ml, and 30–100 ng/ml, respectively.[1]
There is a high prevalence of Vitamin D deficiency in both sunshine deficient and sunshine sufficient countries. It is the most underdiagnosed and undertreated nutritional deficiency throughout the world and the most probable reason for the same is lack of awareness regarding the importance of this Vitamin.[2,3]
Beyond bone integrity, Vitamin D plays a critical role in immune, cardiovascular, endocrine system, neurophysiological, neuromuscular, and cellular differentiation and has anti-cancer actions.[4] Few recent studies have stated that low 25(OH)D is associated with cardiovascular risk factors such as dyslipidemia, hypertension, and diabetes mellitus.[5]
Dyslipidemia is an independent, modifiable, and risk factor for cardiovascular diseases. The rate of dyslipidemia is not only high and increasing in most developed countries, similar trend is now seen in most developing countries as a result of change in diet and lifestyle.
Few studies in the recent past indicate that there is an association between Vitamin D deficiency and elevated serum levels of total cholesterol, low-density lipoprotein cholesterol, and low serum levels of high-density lipoprotein-cholesterol.[6-8]
The current study is being conducted among young medical students as it will provide a two-fold opportunity of targeting a section of the general population and also create awareness among the future health providers of the community.
MATERIAL AND METHODS
A cross-sectional study was conducted in the Department of Physiology, Government Medical College, Kannur, Kerala. The duration of the study was 3 months. It was conducted among 1st year medical students of ACME Pariyaram, Kannur.
All participants gave their informed consent, and both the Institutional Research Committee and the Ethics on Research Committee of Academy of Medical Sciences, Pariyaram, Kannur approved the protocol (No.G1.2747/12/ACME) on 29 September 2018.
Inclusion criteria
The following criteria were included in the study:
Female students of age group 18–20 years.
Subjects who have given informed written consent.
Exclusion criteria
The following criteria were excluded from the study:
Those who were absent and sick on the day of study.
Subjects not willing to participate in the study.
Those suffering from any major illness or on regular drugs.
Study materials and tools
Blood samples were collected after 10–12 h of overnight fasting. Complete fasting lipid profile was measured by photometry method. The biochemical estimation of serum 25-hydroxy 25(OH)D was done using fully automated chemiluminescent immunoassay.
The study included 30 1st year medical and dental female students aged between 18 and 20 years.
Study design: Cross-sectional study.
Study setting: Government Medical College, Kannur, Pariyaram, Kerala.
Study period: Three months, 2018.
Study population: Thirty Medical Undergraduates of Government Medical College, Kannur, Pariyaram.
Statistical analysis
Data were entered into Microsoft Excel spreadsheet 2013. Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) 20 window software (SPSS Inc.). Vitamin D status and lipid profile parameters were compared using Pearson Chi-square test. P < 0.05 was considered as statistically significant. Descriptive statistics such as mean, standard deviation, and inferential statistics like Chi-square test were used. P < 0.05 was considered significant.
RESULTS
Overall, 96.6% of subjects had deficient (<20 ng/mL; 93.3%) or insufficient (20–<30 ng/mL; 3.3%) levels and only 1 student had normal level (30–100 ng/mL; 3.3%) of 25(OH)D. About 40% of these subjects had dyslipidemia.
There is a high prevalence of Vitamin D deficiency, but no significant association found between Vitamin D deficiency and dyslipidemia as shown in Figure 1. Furthermore, there was no significant association between Vitamin D deficiency and individual parameters of dyslipidemia such as TC, LDL, TG, HDL and Non-HDL as shown from Figures 2-6, respectively.

- Bar chart comparing Vitamin D status and dyslipidemia.
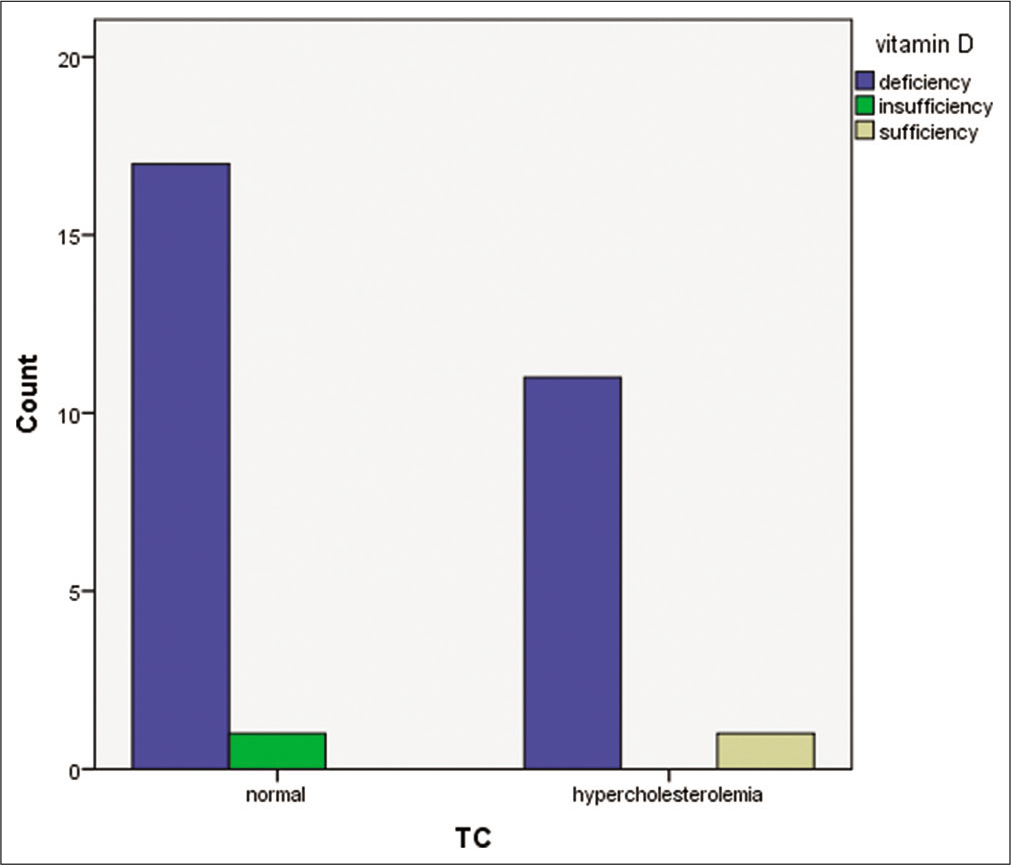
- Bar chart comparing Vitamin D status and total cholesterol level.
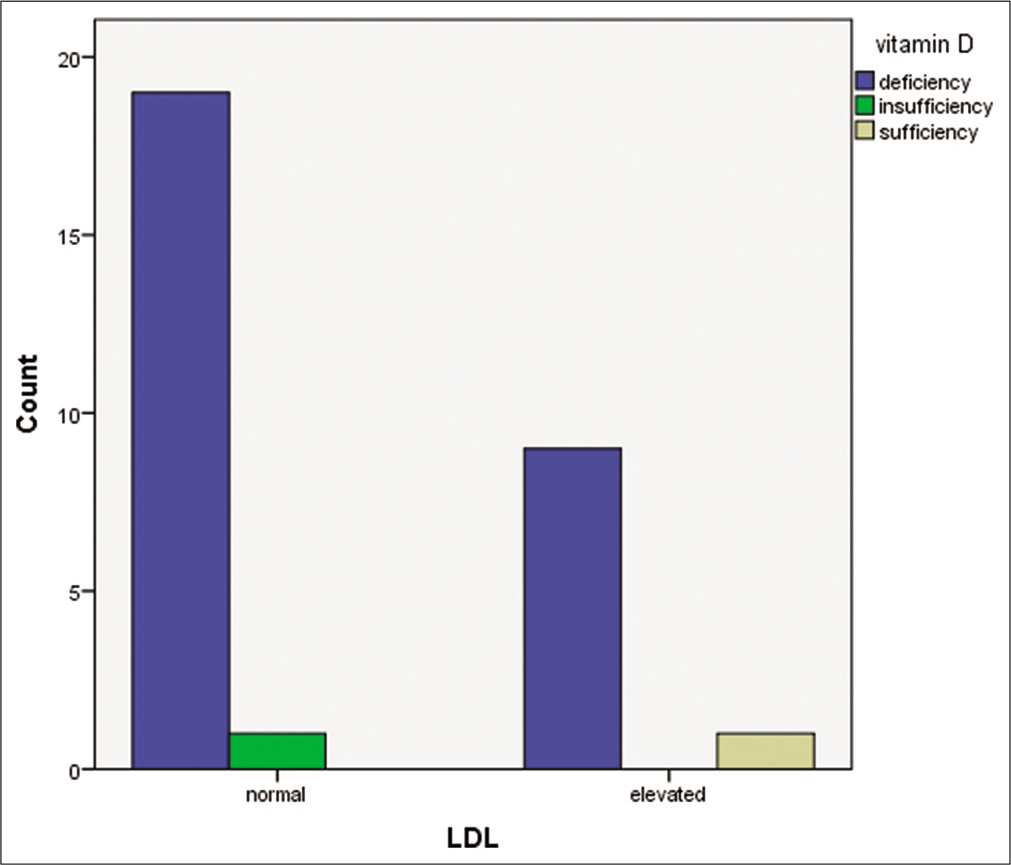
- Bar chart comparing Vitamin D status and low-density lipoprotein.
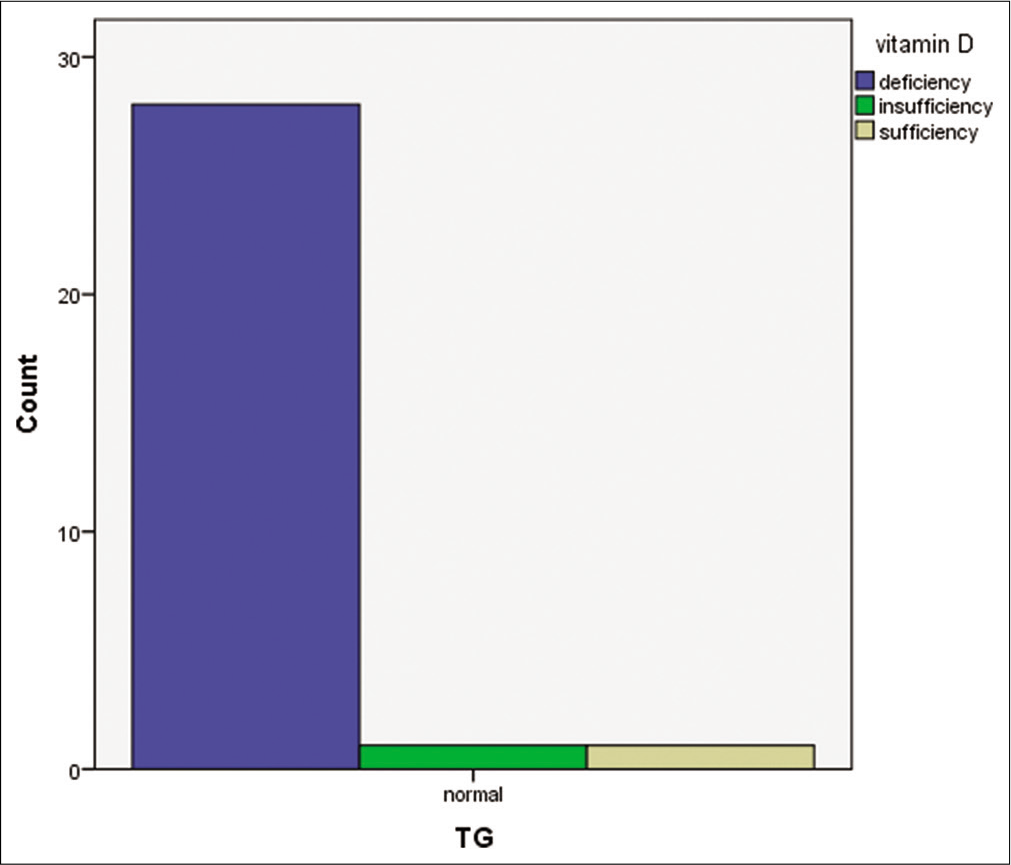
- Bar chart comparing Vitamin D status and triglyceride level.
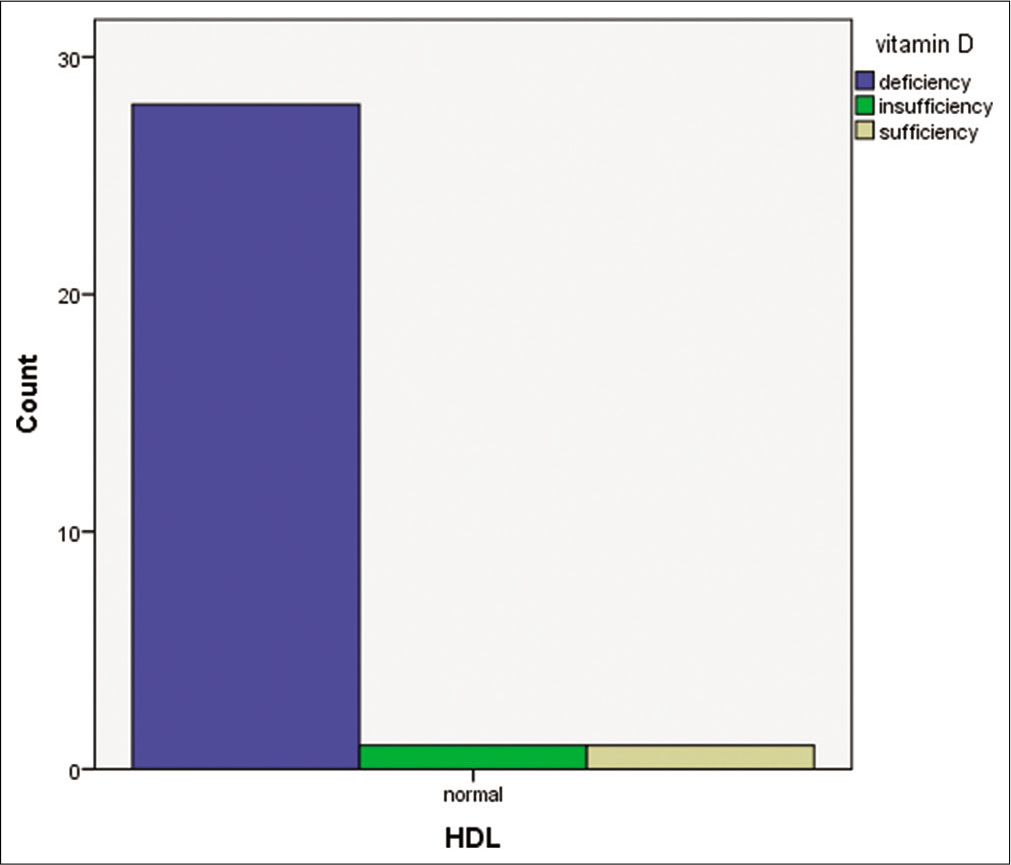
- Bar chart comparing Vitamin D status and high-density lipoprotein level.
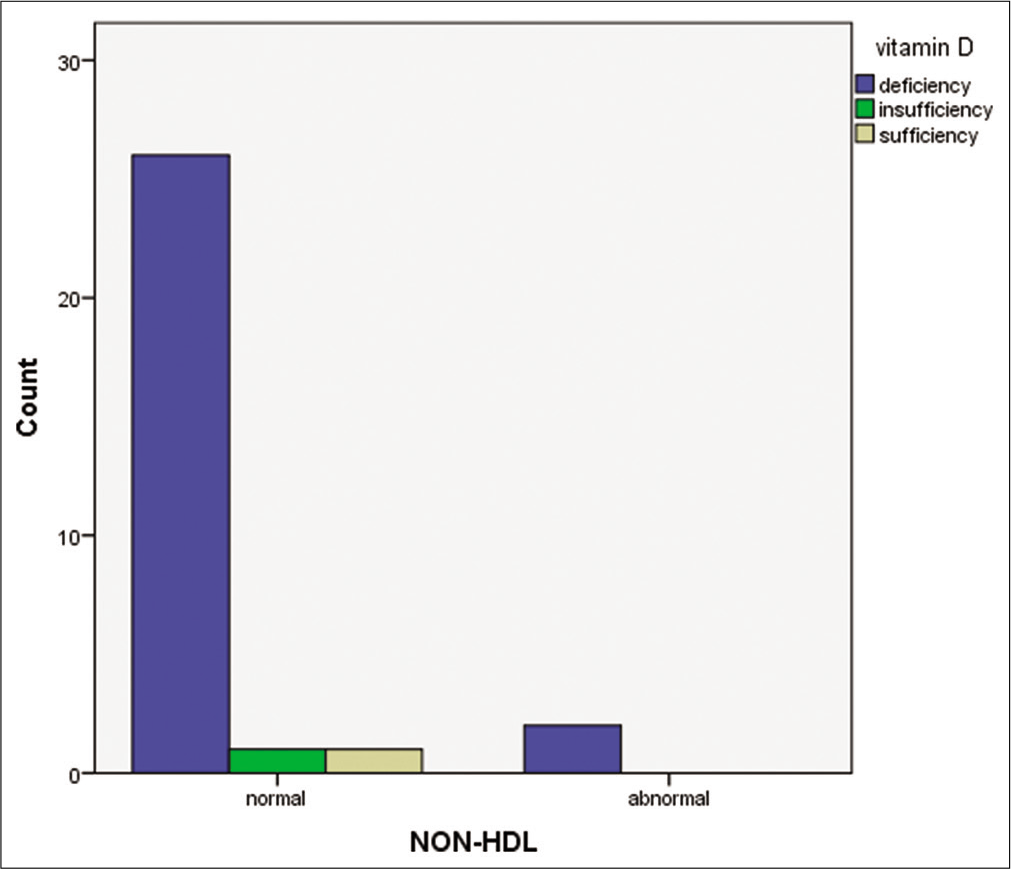
- Bar chart comparing Vitamin D status and non-high-density lipoprotein.
DISCUSSION
Vitamin D deficiency continues to be an unrecognized epidemic in many populations around the world.[3]
In India, several community-based and hospital based studies in the past decade showed a high prevalence of Vitamin D deficiency throughout the country.[4]
Our study demonstrated a very high prevalence of Vitamin D deficiency and conforms to other studies conducted among medical students in different parts of the world.[5]
In contrary to majority of the studies, our study showed no significant association between Vitamin D status and dyslipidemia.[6,7]
Meanwhile, recent few studies suggested that Vitamin D deficiency is associated with changes in serum levels of apolipoproteins, but not with fasting levels of lipids.[8]
Therefore, more studies are needed to confirm the possible effects of Vitamin D on serum concentrations of lipids.
CONCLUSION
It is a paradox that in spite of being a tropical country where there is abundant sunlight, there is a high prevalence of this sun-shine vitamin deficiency. The fast changing lifestyle and sedentary indoor life could be responsible for this deficiency in epidemic proportions. Food, dress, and other cultural practices also play a role, but of less magnitude. While the latter may take time to evolve into remedial level, the former can be changed immediately with a change of attitude by especially the youth of the country. So far as, medical undergraduates are concerned incorporating more of outdoor activities such as sports in the curriculum would address this issue more effectively. Although our study does not show any significant association between serum Vitamin D levels and lipid profile, but several other studies have suggested a negative impact of deficient Vitamin D levels on lipid profile. More studies in this topic with greater study population will give us more evidence on the same.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Evaluation, treatment, and prevention of Vitamin D deficiency: An endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-30.
- [CrossRef] [PubMed] [Google Scholar]
- Worldwide Vitamin D status. Best Pract Res Clin Endocrinol Metab. 2011;25:671-80.
- [CrossRef] [PubMed] [Google Scholar]
- Global Vitamin D status and determinants of hypovitaminosis D. Osteoporos Int. 2009;20:1807-20.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Vitamin D deficiency and associated risk factors among children residing at high altitude in Shimla district, Himachal Pradesh, India. Indian J Endocrinol Metab. 2017;21:178-83.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Vitamin D deficiency and its associated factors among the urban elderly population in Hyderabad metropolitan city, South India. Ann Hum Biol. 2018;45:133-9.
- [CrossRef] [PubMed] [Google Scholar]
- Deficiency of 25-hydroxyvitamin D and dyslipidemia in Indian subjects. J Lipids. 2013;2013:623420.
- [CrossRef] [PubMed] [Google Scholar]
- The association between serum 25-hydroxyvitamin D3 concentration and serum lipids in the rural population of China. Lipids Health Dis. 2017;16:215.
- [CrossRef] [PubMed] [Google Scholar]
- Association between serum level of Vitamin D and lipid profiles in Type 2 diabetic patients in Iran. J Diabetes Metab Disord. 2014;13:7.
- [CrossRef] [PubMed] [Google Scholar]






