Translate this page into:
Comparison of Prevalence of Premenstrual Syndrome Symptoms among Medical and Non-medical Professional Females and its Association with Depression, Anxiety, and Stress: A Cross-sectional Study

*Corresponding author: Farhat Ijaz, Department of Physiology, CMH Lahore Medical College and Institute of Dentistry, Lahore, Pakistan. farhat_khurram_rana@cmhlahore.edu.pk
-
Received: ,
Accepted: ,
How to cite this article: Fazal TB, Razzaq Y, Ijaz F, Razzaq A, Zaheer S, Meral U. Comparison of Prevalence of Premenstrual Syndrome Symptoms among Medical and Non-medical Professional Females and its Association with Depression, Anxiety, and Stress: A Cross-sectional Study. Glob J Med Pharm Biomed Update. 2024;19:7. doi: 10.25259/GJMPBU_99_2023.
Abstract
Objectives:
Premenstrual syndrome (PMS) includes psychological and somatic symptoms that start shortly before a woman’s menstruation. They are shown to affect a woman’s life negatively. Theis study aimed to measure the prevalence of PMS levels among the female population of Pakistan, to check its association with depression, anxiety, and stress, and to get a comparative analysis of PMS symptoms between medical professionals, non-medical professionals, and housewives.
Material and Methods:
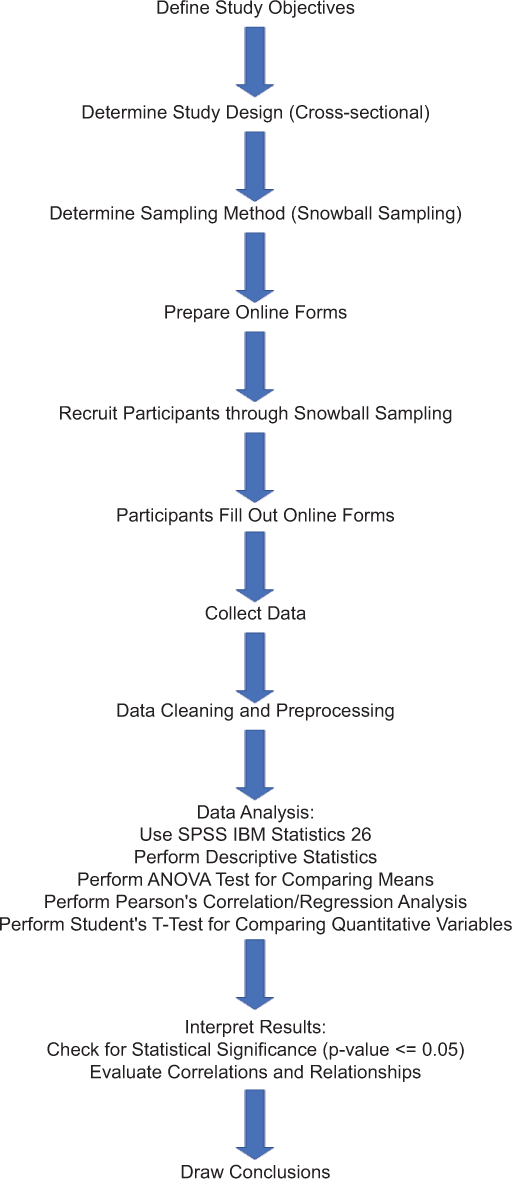
A cross-sectional study was conducted through online forms using snowball sampling on the sample size of n = 431. The questionnaire employed used shortened premenstrual assessment forms to measure the levels of PMS, along with depression, anxiety, and stress scale (DASS) to measure the levels and correlate them. Demographics included the name, age, profession, menstrual cycle regularity, pregnancy, contraception use, menopausal symptoms, and psychiatric disorders of the participants. Data analysis using descriptive statistics was done using the Statistical Package for the Social Sciences IBM Statistics 26. Analysis of variance was performed to compare the means. Pearson’s correlation/regression analysis was done to quantify related variables. Parametric test (Independent T test also called student t test) was used to compare quantitative variables. P ≤ 0.05 was considered statistical significance.
Results:
The majority of participants (58.2%) suffered from mild PMS while 39.9% and 8% of them suffered from moderate and severe PMS symptoms, respectively. Normal scores in DASS criteria were most prevalent among study subjects: (34.6%) anxiety, (53.6%) depression, and (47.8%) stress. Anxiety’s “extreme score” of (94%) was the most prevalent, while stress was the least. PMS was greatest in women working in the medical profession, second only to housewives. Depression and stress were most prevalent among women in medicine. Anxiety was highest among housewives.
Conclusion:
Most of our participants (58.2%) suffered from mild PMS, while severe PMS was present in only (8%) of the subjects. A strong correlation between PMS, depression, anxiety, and stress was found.
Keywords
Premenstrual syndrome
Depression
Anxiety
Stress
INTRODUCTION
Premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) are the psychological events a woman faces during her monthly cycles. These states include psychological, emotional, cognitive, and somatic symptoms that cause significant disablement during the luteal phase, which is the phase starting from ovulation and ending with the hemorrhagic period of the menstrual cycle. The symptoms begin to resolve shortly after bleeding occurs.[1] Premenstrual dysphoric disorder (PMDD) is a severe form of PMS and is added as a mental disorder in The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) definitions.
PMS affects a woman very negatively; it is quite prevalent but often underdiagnosed and underestimated.[2] The core symptoms of PMS and PMDD are anxiety/tension, mood swings, aches, appetite/food cravings, cramps, and decreased interest in activities. Emotional, somatic, and behavior are the three categories into which these symptoms fall.[3] Female adolescents and young adults feel limited in achieving their developmental goals due to PMS, as has been reported.[4]
A study conducted in South India reported the highest educational qualification, occupation, and sexual activity to be significantly associated with PMS, with high prevalence among working women and affecting their quality of life. This study showed that bankers had the highest while healthcare workers had the lowest prevalence of PMS.[5] Similarly, another research proved that stress is a major risk factor for PMS.[6]
PMS may lead to many effects: productivity in the work environment decreases, health-related quality of life is lowered, and interpersonal relationships and everyday activities are affected.[7-9] Athletic and academic performance is negatively impaired.[3,10] Further, cognitive and emotional alterations also occur with PMS.[11]
The pathophysiology behind PMS is unknown but is thought to be a complex interaction between various multi-factorial factors affecting hormonal activities in the body, causing progesterone effects on neurotransmitters such as serotonin, opioids, and catecholamines.[3] There are interactions with genetic lifestyle behaviors, dietary lifestyle, culture, ethnicity, etc.[12]
People use various interventions to manage their symptoms. Pharmacological interventions are used by some, such as selective serotonin reuptake inhibitors (SSRIs) or anxiolytics and oral contraceptive pills (OCPs), while others go for therapies like exercise, dietary modifications, aerobics, cognitive therapies, and massage therapies.[13]
Therefore, our study aims to assess the prevalence of PMS in females in medical and non-medical fields as well as its association with stress, anxiety, and depression caused by workload and other sociodemographic factors. PMS is a poorly researched topic in Pakistan due to cultural reasons and is considered taboo. Our study will help females manage PMS symptoms and improve their quality life.
We included medical students as our study subjects because the medical profession is stressful and associated with longer working hours, fewer rewards, and forces women to be away from family for a major part of the day. This study focused on this population because medical professionals are known to be more aware of the biochemical and physical aspects of PMS and are considered to have better coping skills.
Research in the past was focused on the prevalence of PMS and its impact on the quality of life. Little is known about occupations impacting it. Our research is novel about the idea of PMS association with various professions and explores its correlation with depression, anxiety, and stress.
Aim and objective
Our study aims to estimate and compare the prevalence of PMS symptoms among the medical and non-medical female population as well as correlate it with depression, anxiety, and stress among them.
MATERIAL AND METHODS
This was a cross-sectional study, and the data collection phase was done from January to April 2021. The female population of Pakistan was recruited randomly, in the reproductive age group from 12 years of age to 55, and included housewives and those in medical and non-medical fields so a comparative analysis can be obtained. The sample size of 431 was determined by utilizing Cochran’s formula with a confidence interval of 95% and a 6% margin of error. Furthermore, a non-probability convenient sampling technique was used. Participants who fulfilled the inclusion criteria participated in the study.
The study was conducted at a medical college in Pakistan and approval was obtained from the Ethics Committee of the Institute. The study population was randomly selected through online survey techniques using Email, Facebook, and WhatsApp. The target population was the females in Pakistan. The same English version in Google Forms was used for both the scales shortened premenstrual assessment form (SPAF) and depression, anxiety, and stress scale (DASS)-21. Housewives spoke English because the target population was mostly urban. The snowball sampling technique was applied The females included in the reproductive age group were the ones having a regular menstral cycle for 2 months. Participants who were pregnant and post-menopausal were excluded from the study; those with pre-existing psychiatric illnesses such as anxiety disorder depressive disorder and those on psychiatric treatment were also exclued.
Online surveys were used to collect the data. The questionnaire was divided into three parts: sociodemographic information, the SPAF, and the DASS-21 criteria. The survey form was shared through Google Forms, other online and social media platforms, and email. Sociodemographic data included the participants’ name (if comfortable sharing), age, profession (housewife, medical professional, and non-medical person), menstrual cycle regularity, pregnancy (if present), contraceptive pill or hormonal method use, no menopausal symptoms, and psychiatric disorder (if present).
We employed SPAF, which includes both somatic and behavioral symptoms of PMS. It has ten questions, which are rated based on a 6-point Likert scale: 1 (not present or no change from usual) and 6 (extreme change, noticeable even to casual acquaintances). The participants were then divided into three categories based on their score: Mild symptoms, with a score of <30; moderate symptoms, with a score between 30 and 50; and severe symptoms, with a score >50.[14] The SPAF provides the same assessment as the original 95-item premenstrual assessment form, as demonstrated by its equally strong reliability (test-retest coefficient range of 0.6– 0.7) and validity (internal consistency coefficient of 0.95).[15]
The DASS-21 Items was used for measuring depression, anxiety, and stress.[13] It has a total of three sets, each with seven items and further subscales, one each for depression, anxiety, and stress, and measures the emotional state through self-reporting. The depression scale assesses dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest/involvement, anhedonia, and inertia. The anxiety scale assesses autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect. The stress scale is sensitive to levels of chronic non-specific arousal. It assesses difficulty relaxing, nervous arousal, being easily upset/agitated, irritable/over-reactive, and impatient. The reliability of the DASS-21 has been proven in many studies, including the ones conducted in the English-speaking respondents from the United States, Australia and Ghanian students and Ghanaian participants, was excellent (coefficient alpha = 0.93 and 0.95, respectively).[16]
Both questionnaires were employed at random times in the populations’ cycle, with no specification of time or measured retrospection, and were based on recall of how they felt through their cycle on average.
Calculations were, then, made by adding the individual scores of relevant items. Depression score is categorized as normal 0–9, mild 10–13, moderate 14–20, severe 21–27, and extremely severe 28+. Anxiety as normal 0–7, mild 8–9, moderate 10–14, severe 15–19, and extremely severe 20+. Stress has the categories 0–14 normal, 15–18 mild, 19–25 moderate, 26–33 severe, and 34+ extremely severe.[17]
Data analysis was done using the Statistical Package for the Social Sciences IBM Statistics 26. The study’s outcome variables were described using descriptive statistics. An analysis of variance (ANOVA) test was performed to compare the means. Pearson’s correlation/regression analysis was used to quantify related variables. Student t-test was used to compare quantitative variables. P ≤ 0.05 was considered statistical significance [Flow Chart].
Approval for the study was sought by the Ethical Review Committee of the CMH Lahore Medical College and Institute of Dentistry (59/ERC/CMHLMC). Informed consent of the participants was obtained and their identities were kept anonymous. There were no conflicts of interest, and participants were not given any incentives.
FLOW CHART
RESULTS
Inclusion criteria were met by a total of 431 women; pregnant and post-menopausal women were excluded, which, in our population, were 1 and 2, respectively. Candidates fell in the ages ranging from 15 years to 46 years, 323 (74.9%) falling in the category of 21–29 years of age, and the mean of the ages was 22.345 (Standard deviation 0.1633). Three hundred and thirteen of the participants belonged to a medical profession, 99 to a non-medical profession, and 19 were housewives. Of the 431 women, 390 (90.5%) had a regular menstrual cycle, 417 (96.8%) were not using any contraceptive, and 20 (4.64%) had a pre-diagnosed psychiatric disorder present.
The majority of participants suffered from mild PMS (58.2%), while 39.9% and 8% of them suffered from moderate and severe PMS symptoms, respectively. Normal scores in DASS criteria were most prevalent among study subjects: (34.6%) anxiety, (53.6%) depression, and (47.8%) stress. The point to note here is that anxiety’s “extreme score” of 94% was the most prevalent while stress was the least [Tables 1 and 2].
| SPAF/PMS Severity | n (%) |
|---|---|
| Mild | 251 (58.2) |
| Moderate | 172 (39.9) |
| Severe | 8 (1.9) |
PMS: Premenstrual syndrome, SPAF: Shortened premenstrual assessment form, n: Number of participants Frequency
| Severity | Depression n (%) | Anxiety n (%) | Stress n (%) |
|---|---|---|---|
| Mild | 53 (12.3) | 53 (12.3) | 64 (14.8) |
| Moderate | 103 (23.9) | 98 (22.7) | 75 (17.4) |
| Severe | 57 (13.2) | 37 (8.6) | 57 (13.2) |
| Extreme severe | 65 (15.1) | 94 (21.8) | 29 (6.7) |
n: number of participants: Frequency
ANOVA test was performed for the comparison of mean values of PMS and depression, anxiety, and stress scores. There was a significant difference based on profession between medical and non-medical working women and housewives stress scoring at P = 0.025. There was, however, no statistically significant difference in the rest of the scores [Table 3].
| Outcome | Medical (mean) | Non-medical (mean) | Housewife (mean) | t value | P-value | 95% CI |
|---|---|---|---|---|---|---|
| PMS score | 27.7540 | 24.7576 | 27.8947 | 1.643 | 0.061 | −26.0215,28.1224 |
| Depression score | 15.2780 | 14.3434 | 14.3158 | 0.619 | 0.732 | −13.9616,16.0601 |
| Anxiety score | 11.6741 | 11.9394 | 12.7368 | −0.495 | 0.867 | −10.9250,12.6388 |
| Stress score | 16.9393 | 13.7980 | 14.4211 | 0.012 | 0.025 | −15.1185,17.0950 |
PMS: Premenstrual syndrome, CI: Confidence interval
PMS was greatest in medical women, second only to housewives. Depression and stress were most prevalent among medical women. Anxiety was highest among housewives.
There was a strong correlation, as indicated by the “r” value, between PMS and depression, anxiety, and stress [Table 4]. Stress had the highest, while anxiety had the lowest correlation; depression was found to be somewhere in the middle. In 46.8% of the participants, PMS was found to be due to stress, whereas in 38.2%, PMS was due to depression. Meanwhile, 30.4% of the participants had PMS that was due to anxiety. The correlation coefficients between PMS and all disorders were strongly significant (<0.01).
| PMS (r) | (r) 2 | P-value | |
|---|---|---|---|
| Depression | 0.618 | 38.2% | 0.000 |
| Anxiety | 0.552 | 30.4% | 0.000 |
| Stress | 0.684 | 46.8% | 0.000 |
PMS: Premenstrual syndrome, (r) represents the value of the Pearson correlation coefficient, which is used to note strength and direction amongst variables, whereas (r)2 represents the coefficient of determination, which determines the strength of a model.
In terms of psychiatric condition present, the PMS was only 0.8% related, and the P-value was not significant, similar to the use of contraception. It was, however, observed that women using contraception had lower PMS symptoms than non-users. The women who had a psychiatric disorder present had more PMS symptoms than those who did not based on the comparison of the mean values.
DISCUSSION
This study estimated how common the presence of PMS is among women of three different backgrounds; grossly divided into medical working life, non-medical life, and those who stay at home as housewives. It also investigated the correlation of PMS with depression, stress, and anxiety faced by women in their working lives, as well as compared the data of women using contraception and the presence of a psychiatric disorder and whether it affected PMS levels in them.
Most of our participants (58.2%) suffered from mild PMS, while severe PMS was present in only (8%) of the subjects. Our results were consistent with the study conducted in Riyadh to measure the prevalence of PMS among female students of medical and non-medical colleges,[2] where also only (8%) of the subjects had severe PMS and (59.4%) had moderate PMS. Similarly, another study that was conducted in Turkey found 47% and 5.8% of medical students to have moderate and severe PMS, respectively.[9] Our results also align with a study conducted in Saudi Arabia.[18]
Our study used DASS scoring to determine depression, anxiety, and stress levels. Depression scores were almost similar in non-medical professional women and housewives but varied slightly from medical professional women having higher mean scores.[17,19] Anxiety levels were almost similar in medical and non-medical women but greater in housewives (mean 12.73). Stress scores varied significantly, with the highest mean value in medical women (16.93), non-medical the least while housewives intermediate. Keeping with it, the study, which compared prevalence among female students of Riyadh, non-medical students had higher mean scores, (7.12) for depression and (8.29) for stress. In comparison, medical students had a mean score of (5.88) for depression and (6.91) for stress.[2] Another study by Al Ahsas’s also used DASS to measure depression, anxiety, and stress prevalence; the study found that depression was 27%, anxiety 40.4%, and stress 31.5% among students diagnosed with PMS.[19]
In terms of the association of PMS with depression, anxiety, and stress, a positive correlation was found. Results were consistent with the Riyadh study.[2] PMS and stress, having an r-value of 0.684, had the highest correlation. PMS with depression had an r-value of 0.618, which came somewhere in between, while anxiety had the lowest correlation, with an r-value of 0.552. Hence, the finding highlights the repercussions of PMS and why it should be addressed.
Most previous studies have focused on the prevalence of PMS, while ours not only gave an understanding of its association with stress, anxiety, and depression but also found the relationship between the use of contraception and psychiatric disorders present previously in women. A psychiatric disorder makes a woman more prone to suffering from PMS. The use of contraception had a slight reduction in PMS symptoms, which means that this could be used as a management modality in the sufferers. There is a lack of consensus in the literature on the best management options for PMS.
Among the limitations we faced the first was the fact that women were at different stages of their menstrual cycle; and because they were supposed to recall their symptoms, this could result in recall bias. Secondly, the sample was highly selective; therefore, future studies should focus on a a more generalized population and should gather data for over a longer duration in a woman’s cycle.
Implications for practice and/or policy
PMS does not only have psychological implications, but it also affects physical health as well. Apart from biomedical explanations for it, many biological reasons can be sought, too. As is evident from the study, this topic is not thoroughly addressed, leading to a decline in occupational productivity and health-related quality of life. Hence, reproductive health topics should be started in the early years as part of educational programs. Specialized clinics should ensure better counseling for women seeking help for PMS. These steps will help raise awareness and will become a stepping stone in developing proper guidelines for better detection and management. This will also help reduce reluctance among people in general when talking about PMS.
CONCLUSION
PMS is not rigorously researched and addressed as an issue, even though it is quite common. Yet, it not only hinders physical health but also has psychological implications. Better counseling at specialized clinics should be given, which can help reduce the barrier to seeking management or psychological help. Future studies should focus more on the risk factors involved, so that PMS can be tackled at its root.
Ethical approval
The research/study approved by the Institutional Review Board at CMH Lahore Medical and Institute of Dentistry Ethical Review Committee, number 59/ERC/CMHLMC, dated January 10, 2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Premenstrual Syndrome, and Premenstrual Dysphoric Disorder. Am Fam Physician. 2016;94:236-40.
- [Google Scholar]
- Prevalence of Premenstrual Syndrome Levels and Its Management among Female Students Of Medical and Non-medical Colleges in Riyadh. Cureus. 2020;12:e11595.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence, Impacts and Medical Management of Premenstrual Syndrome among Female Students: Cross-sectional Study in College of Health Sciences, Mekelle University, Mekelle, Northern Ethiopia. BMC Womens Health. 2014;14:52.
- [CrossRef] [PubMed] [Google Scholar]
- Premenstrual Syndrome is Associated with Dietary and Lifestyle Behaviors Among University Students: A Cross-sectional Study from Sharjah, UAE. Nutrients. 2019;11:1939.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Premenstrual Syndrome and Its Effect on Quality of Work Life in Working Women in South India. Ind Psychiatry J. 2023;32:255-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Premenstrual Syndrome among Students-Stress a Potential Risk Factor. Clin Epidemiol Global Health. 2023;23:101368.
- [CrossRef] [Google Scholar]
- The Effect of Premenstrual Symptoms on Activities of Daily Life. Fertil Steril. 2010;94:1059-64.
- [CrossRef] [PubMed] [Google Scholar]
- Health and Economic Impact of the Premenstrual Syndrome. J Rep Med. 2003;48:515-24.
- [Google Scholar]
- Premenstrual Syndrome in Turkish Medical Students and Their Quality of Life. J Obstet Gynaecol. 2015;35:275-8.
- [CrossRef] [PubMed] [Google Scholar]
- Premenstrual Syndrome and Premenstrual Dysphoric Disorder in Japanese Collegiate Athletes. J Pediatr Adolesc Gynecol. 2015;28:215-8.
- [CrossRef] [PubMed] [Google Scholar]
- Emotional Interference and Attentional Processing in Premenstrual Syndrome. J Behav Ther Exp Psychiatry. 2017;54:77-87.
- [CrossRef] [PubMed] [Google Scholar]
- Menstrual Patterns and Disorders among Secondary School Adolescents in Egypt. A Cross-sectional Survey. BMC Womens Health. 2015;15:70.
- [CrossRef] [PubMed] [Google Scholar]
- A Review of Treatment of Premenstrual Syndrome and Premenstrual Dysphoric Disorder. Psychoneuroendocrinology. 2003;28(Suppl 3):39-53.
- [CrossRef] [PubMed] [Google Scholar]
- Stress, Quality of Life and Physical Activity in Women with Varying Degrees of Premenstrual Symptomatology. Women Health. 2004;39:35-44.
- [CrossRef] [PubMed] [Google Scholar]
- The Depression Anxiety Stress Scale 8-items Expresses Robust Psychometric Properties as an Ideal Shorter Version of the Depression Anxiety Stress Scale 21 among Healthy Respondents from Three Continents. Front Psychol. 2022;13:799769.
- [CrossRef] [PubMed] [Google Scholar]
- The Depression, Anxiety and Stress Scale (DASS-21) as a Screener for Depression in Substance Use Disorder Inpatients: A Pilot Study. Eur Addict Res. 2017;23:260-8.
- [CrossRef] [PubMed] [Google Scholar]
- Manual for the Depression Anxiety Stress Scales. Sydney: The Psychology Foundation 1995
- [CrossRef] [Google Scholar]
- The Phenomenology of Premenstrual Syndrome in Female Medical Students: A Cross Sectional Study. Pan Afr Med J. 2010;5:4.
- [CrossRef] [PubMed] [Google Scholar]







