Translate this page into:
Comparative Effect of Escitalopram and Citalopram on Depressive Symptoms of Patients with Schizophrenia: A Double-Blind Randomized Controlled Trial
*Corresponding author: Sussan Moudi, Social Determinants of Health Research Center, Health Research Institute, Babol University of Medical Sciences, Babol, Iran. sussan.mouodi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Hamzehpour R, Mohammadkhani M, Khafri S, Moudi S. Comparative effect of escitalopram and citalopram on depressive symptoms of patients with schizophrenia: A double-blind randomized controlled trial. Glob J Med Pharm Biomed Update 2022;17:20.
Abstract
Objectives:
Given the importance of the management of depression in patients with schizophrenia, this research was carried out to compare the therapeutic effects of escitalopram and citalopram on depressive symptoms of these patients.
Material and Methods:
This double-blind randomized controlled trial was conducted on 60 patients diagnosed with schizophrenia. The patients who had depression based on the Calgary Depression Scale for Schizophrenia (CDSS) were included in the study. The first group received 10–40 mg/day of citalopram, and the second group received 5–20 mg/day of escitalopram. The patients were treated for 8 weeks. Any reduction in depressive symptoms based on the CDSS measure was considered the primary outcome of the research.
Results:
Although the two groups had no significant difference in CDSS score at the initial assessment (P = 0.86), after 8 weeks, the depressive symptoms decreased and a significant difference was observed between the two groups (P = 0.03). The two groups had no significant difference in drug side effects, except for anorexia (P = 0.03).
Conclusion:
Depressive symptoms decreased significantly after 8 weeks of treatment with both citalopram and escitalopram; however, these symptoms had more reduction in patients taking escitalopram than the individuals receiving citalopram.
Keywords
Schizophrenia
Depression
Citalopram
Escitalopram
INTRODUCTION
Schizophrenia is a serious neurodevelopmental psychiatric disorder characterized by impaired thought process and cognition, poor emotional responsiveness, abnormal social behaviors, and other negative symptoms. Its early management needs more consideration, as the clinical manifestations of this disorder typically occur in late adolescence or early adulthood, and most patients experience notable disability and lose their educational and social interaction and functioning throughout the illness.[1,2] The World Health Organization reported the worldwide point prevalence of schizophrenia as 20 million people,[3] and its lifetime prevalence has been estimated as near 1%.[2]
Three stages of disease including the prodromal, active, and residual phase have been described for schizophrenia. Depression has been represented as common comorbidity in these patients.[4] Depressive symptoms can be observed in 70–80% of individuals with schizophrenia, and almost 50% of these patients experience depressive symptoms during the first episode or in the prodromal stage. Patients and family members may not pay attention to depression; and sometimes, depression can be misdiagnosed with negative symptoms of schizophrenia.[5] The occurrence of depression in these patients can worsen the person’s disability. Depressive symptoms often lead to severe impairment in daily functioning, reduced quality of life, and increased risk of suicide and leading to a frequent need for hospitalization in patients with schizophrenia.[4,6] Furthermore, people with coincident schizophrenia and depression are more likely to have recurrent psychiatric problems, or be involved with alcohol and substance use disorders.[7]
Recent evidence demonstrated an association between volume loss of the hippocampus in the early stages of schizophrenia and poor clinical outcomes in these patients and recommended antidepressants for reduction of this volume loss. It has been shown that antidepressants can affect the hippocampus through different mechanisms such as the release of brain-derived neurotrophic factors.[8] Schizophrenia patients with antipsychotic treatment who receive antidepressants have a lower rate of major depressive disorder than patients with antipsychotic treatment without antidepressants.[5]
Selective serotonin reuptake inhibitors (SSRIs) such as citalopram and escitalopram have been prescribed to improve the negative and depressive symptoms of schizophrenia; however, the data on the effectiveness and side effects of these medications in patients diagnosed with schizophrenia are limited.[9-13] These drugs have minimal pharmacokinetic interaction with antipsychotics and may improve the severity of negative symptoms in patients with schizophrenia.[8] This research was conducted to compare the therapeutic effects of escitalopram and citalopram on depressive symptoms of patients with schizophrenia.
MATERIAL AND METHODS
Study design and setting
This double-blind randomized controlled trial was carried out with parallel groups, without a control group on patients with a diagnosis of schizophrenia referred to the psychiatric clinics of Babol University of Medical Sciences, Iran. Blinding was conducted by the research statistical consultant; therefore, neither the clinician nor the patient knew what medicine was prescribed. Patients were matched into the two groups in terms of the severity of schizophrenia.
Participants
Inclusion criteria were diagnosis of schizophrenia based on DSM-V criteria through a structured clinical interview by a psychiatrist (faculty member and resident of psychiatry) and diagnosis of depression based on the Calgary Depression Scale for Schizophrenia (CDSS).
Exclusion criteria were substance abuse, any serious medical disorders such as epilepsy, ischemic heart disease, heart failure, intellectual disability, Parkinson’s, and severe mood or cognitive disorders.
Interventions
The first group of patients was treated with citalopram (manufactured by Ramofarmine Drug Company, Iran). The treatment was started with a dose of 10 mg at night and increased up to 40 mg/day based on the response to treatment.
The second group received escitalopram (manufactured by Abidi Drug Company, Iran) starting at a dose of 5 mg at night and increased up to 20 mg/day considering the response to treatment.
The patients were treated for 8 weeks.
Outcomes and variable assessment
Demographic characteristics including age, gender, occupation, marital status, and level of education were collected at the baseline visit, before initiation of the intervention. All patients were followed up 4 and 8 weeks after the treatment. The primary outcome was any reduction in depressive symptoms based on the CDSS measure. The secondary outcome was drug side effects which were collected with a checklist.
CDSS is a 9-item questionnaire that examines the level of depression in people with schizophrenia.[14,15] Due to the presence of symptoms such as decreased energy and concentration, and abnormal sleep in patients with schizophrenia, these characteristics should not be considered for assessing depression in schizophrenia; and CDSS is a proper measure for this purpose. CDSS scores range from 0 to 27. A score higher than 6 was considered for the presence of depression in the patient.[16]
Sample size
Considering a study power of 0.8 and a confidence level of 0.95, the sample size was calculated as 60 patients (30 in each group).
Randomization
The patients were allocated randomly to one of the two intervention groups. The participant’s allocation sequence in two groups was determined by the project statistical consultant with a randomizer software. Opaque-sealed sequentially numbered envelopes (with abbreviated names of A and B for each treatment group) were given to the clinicians for allocation concealment.
Trial registration
This research was registered on the website of the Iranian Registry of Clinical Trials (www.irct.ir) as IRCT20190525043700N1 identification number.
Statistical methods
Data analysis was performed using the SPSS-18 software package. Chi-square, t-test, and analysis of variance repeated measures were used for data analysis. P < 0.05 was considered the significant level.
Ethics approval and consent to participate
All participants provided a written informed consent form at the beginning of the research. The study protocol was approved by the Ethics Committee of Babol University of Medical Sciences with reference code: IR.MUBABOL.HRI.REC.1397.293.
RESULTS
Totally, 60 patients (33 males and 27 females) with schizophrenia and depressive disorder completed the research. The flow diagram of the participants is presented in [Figure 1].
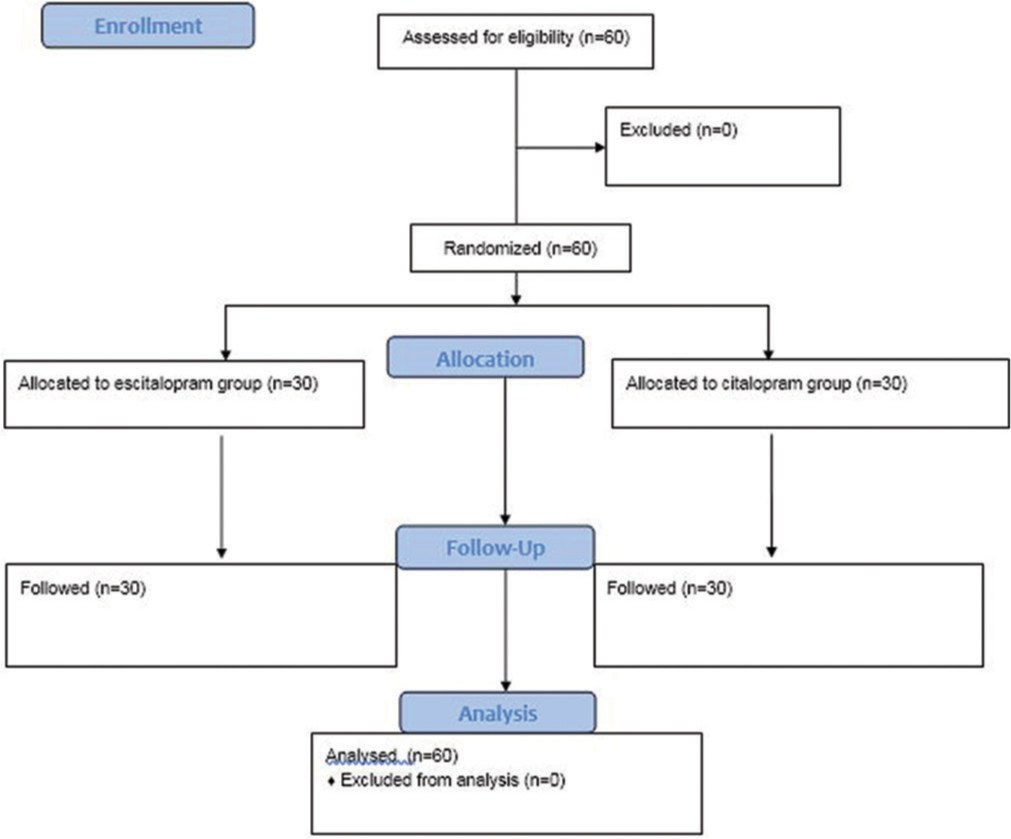
- Flow diagram of the participants.
The baseline characteristics of the participants are presented in [Table 1]. This table shows that the two groups had no significant difference about age (P = 0.33), gender (P = 0.79), and other demographic characteristics (P > 0.05).
| Characteristics | Treatment groups | P-value (Chi-square test) | |
|---|---|---|---|
| Citalopram (n=30) Number (percent) | Escitalopram (n=30) Number (percent) | ||
| Gender | |||
| Male | 17 (56.7) | 16 (53.3) | 0.79 |
| Female | 13 (43.3) | 14 (46.7) | |
| Marital status | |||
| Not-married | 12 (40.0) | 13 (43.3) | 0.79 |
| Married | 18 (60.0) | 17 (56.7) | |
| Years of education (year) | |||
| <6 | 7 (23.4) | 5 (16.6) | 0.81 |
| 6–12 | 13 (43.3) | 14 (46.7) | |
| >12 | 10 (33.3) | 11 (36.7) | |
| Occupation | |||
| Occupied | 15 (50.0) | 10 (33.3) | 0.19 |
| Non-occupied | 15 (50.0) | 20 (66.7) | |
| Age (Mean±SD) | 41.23±4.36 | 42.47±5.39 | 0.33 |
The score of depression at baseline examination, the 4th and 8th weeks after the intervention, is presented in [Table 2]. This table shows that although the two groups had no significant difference in CDSS score at the initial assessment (P = 0.86), after 8 weeks, this difference was significant (P = 0.03). In addition, a declining trend in depression scores was observed in both groups from the start point to the end of the 8th week of treatment (P < 0.001).
| Treatment group | CDSS score (Mean±SD) | P-value | ||
|---|---|---|---|---|
| Before treatment | The 4thweek | The 8th week | ||
| Citalopram | 11.57±1.59 | 10.80±1.44 | 9.87±1.47 | <0.001 |
| Escitalopram | 11.50±1.43 | 10.57±1.56 | 9.03±1.52 | <0.001 |
| P-value | 0.86 | 0.55 | 0.03 | - |
CDSS: Calgary depression scale for schizophrenia
The association of depression score at the end of the study (the 8th week) with the demographic characteristics of the participants showed no significant difference between the two groups [Table 3].
| Characteristics | Treatment groups (Mean±SD of CDSS score) | P-value | |
|---|---|---|---|
| Citalopram (n=30) | Escitalopram (n=30) | ||
| Gender | |||
| Male | 9.88±1.53 | 9.19±1.32 | 0.17 |
| Female | 9.85±1.46 | 8.86±1.74 | 0.12 |
| P-value | 0.94 | 0.56 | - |
| Marital status | |||
| Not-married | 9.75±1.76 | 8.85±1.72 | 0.20 |
| Married | 9.94±1.30 | 9.18±1.38 | 0.10 |
| P-value | 0.73 | 0.56 | - |
| Years of education (year) | |||
| <6 | 9.71±1.97 | 9.80±1.30 | 0.93 |
| 6–12 | 10.0±1.15 | 8.86±1.74 | 0.06 |
| >12 | 9.80±1.61 | 8.91±1.30 | 0.17 |
| P-value | 0.91 | 0.48 | - |
| Occupation | |||
| Occupied | 9.67±1.29 | 8.90±1.44 | 0.17 |
| Non-occupied | 10.07±1.66 | 9.10±1.58 | 0.09 |
| P-value | 0.46 | 0.74 | - |
CDSS: Calgary depression scale for schizophrenia
The findings showed no significant difference in drug side effects, except for anorexia (P = 0.03), between the two study groups [Table 4]. Four (13.3%) of patients receiving citalopram reported anorexia; however, no patient reported this side effect in the escitalopram group.
| Reported drug side-effects | Treatment groups Number (Percent) | P-value (Chi-square test) | |
|---|---|---|---|
| Citalopram (n=30) | Escitalopram (n=30) | ||
| Nausea | 8 (26.7) | 11 (36.7) | 0.40 |
| Diarrhea | 1 (3.3) | 5 (16.7) | 0.08 |
| Dry mouth | 3 (10.0) | 3 (10.0) | 1.0 |
| Excessive sweating | 1 (3.3) | 1 (3.3) | 1.0 |
| Insomnia | 0 | 3 (10.0) | 0.07 |
| Drowsiness | 1 (0.3) | 0 | 0.31 |
| Nightmares | 0 | 1 (3.3) | 0.31 |
| Headache | 1 (3.3) | 3 (10.0) | 0.30 |
| Decreased libido | 2 (2.7) | 2 (2.7) | 1.0 |
| Anorexia | 4 (13.3) | 0 | 0.03 |
DISCUSSION
The present study was performed to compare the effectiveness of citalopram and escitalopram in patients with schizophrenia and depressive symptoms. The findings showed no significant difference in depression between the two groups 4 weeks after the intervention. However, after 8 weeks, patients who received 5–20 mg/day escitalopram had fewer depressive symptoms than people receiving 10–40 mg/day citalopram. Furthermore, in both groups, depressive symptoms decreased significantly over time. Similar to our finding, Stryjer et al. showed that patients with schizophrenia who received escitalopram at a dose of 10– 20 mg/day represented a significant improvement in the total score of depression during 12 weeks of intervention compared with patients who received routine antipsychotic medications.[17] Kamińska et al. recommended coadministration of risperidone and escitalopram for improvement of depressive symptoms and cognitive functions in patients with schizophrenia.[18] Marcus et al. demonstrated that escitalopram, but not citalopram, enhanced cortical dopamine output and N-methyl-D-aspartate receptor-mediated transmission and concluded that adjunct treatment with escitalopram might be effective to improve depressive symptoms in schizophrenia, without increased extrapyramidal side effects.[19] Hinkelmann et al. reported no effect of adjunctive antidepressant treatment on negative symptoms of schizophrenia.[20] A systematic review and meta-analysis revealed that antidepressants might be effective for the treatment of depression in schizophrenia; however, current evidence is mixed and most of the related studies have a small sample size or do not have a high-quality methodological design.[21]
In our research, citalopram and escitalopram could improve depressive symptoms without any serious side effects. Similar to this finding, a recent systematic review and meta-analysis demonstrated the safety of antidepressants in schizophrenia, in combination with antipsychotic drugs.[21]
Sex, marital status, years of education, and occupation had no association with the improvement of depressive symptoms in patients receiving citalopram or escitalopram. Demographic characteristics (such as older age, female gender, and unemployment), substance use disorders, somatic and biological disturbances, and lower treatment adherence can influence the frequency of depressive symptoms in patients with schizophrenia.[4] It seems that similar demographic features in the two study groups resulted in similar treatment outcomes in these two groups.
We could not find similar studies that compared the antidepressant effect of citalopram and escitalopram in patients with schizophrenia. The previous studies considered different end-point for the reduction of depressive symptoms or used different tools for the assessment of depression in patients with schizophrenia, and these characteristics impact on the research findings.[21]
Depression in schizophrenia may be different from unipolar depression, and more specific treatment considerations are needed. Furthermore, individual SSRIs have different properties, for example, the anti-inflammatory effect of citalopram might have some effects in patients with schizophrenia.[21]
Depression can have a significant and seriously negative impact on the prognosis of schizophrenia and deteriorates clinical and functional consequences of the disease independent of psychotic symptomatology.[4] Less than half of patients with comorbid schizophrenia and major depressive disorder receive antidepressants, and nearly half of the patients treated with antidepressants remain unremitted. It means that three out of four patients with the major depressive disorder do not receive successful treatment.[4] The administration of escitalopram for 8 weeks or longer is recommended to improve depressive symptoms in patients diagnosed with schizophrenia, especially for individuals at the early stages of the disease.
The most important strong point of this study was its novelty in comparing the effectiveness and safety of citalopram and escitalopram in patients with schizophrenia. We did not match the consumption of other drugs, such as antipsychotics; also, we did not consider the duration of schizophrenia in this study. These points can be presented as limitations of the research. Further studies with more patients and longer follow-ups are recommended for future interventional studies.
CONCLUSION
In patients with a diagnosis of schizophrenia, depressive symptoms decreased significantly after 8 weeks of treatment with both citalopram and escitalopram; however, the patients who received escitalopram had fewer depressive symptoms than the individuals receiving citalopram. Both citalopram and escitalopram had no serious drug side-effect.
Acknowledgment
The financial support of Babol University of Medical Sciences is appreciated.
Data availability statement
The academic researchers who need the data set associated with the paper can send an email to the corresponding author and ask for the related data.
Authors’ contributions
All authors contributed to the concept and design of the study, acquisition of data, analysis, and interpretation of data.
S.M. drafted the article and all authors revised it critically for important intellectual content; final approval of the version to be published, and aptitude to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Babol University of Medical Sciences, Iran supported this research.
Conflicts of interest
There are no conflicts of interest.
References
- The burden of disease in early schizophrenia-a systematic literature review. Curr Med Res Opin. 2021;37:109-21.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in the incidence and DALYs of schizophrenia at the global, regional and national levels: Results from the global burden of disease study 2017. Epidemiol Psychiatr Sci. 2020;29:e91.
- [CrossRef] [PubMed] [Google Scholar]
- Schizophrenia: Key facts. 2019. Available from: https://www.who.int/news-room/fact-sheets/detail/schizophrenia [Last accessed on 2019 Oct 04]
- [Google Scholar]
- Comorbid major depressive disorder in schizophrenia: A systematic review and meta-analysis. Schizophr Bull. 2021;47:298-308.
- [CrossRef] [PubMed] [Google Scholar]
- Kaplan and Sadock's Comprehensive Text book of Psychiatry (10th ed). Philadelphia, PA: Wolters Kluwer; 2019.
- [Google Scholar]
- Co-morbidity between major depression and schizophrenia: Prevalence and clinical characteristics. Psychiatr Danub. 2020;32:78-83.
- [CrossRef] [PubMed] [Google Scholar]
- The link between schizophrenia and substance use disorder: A unifying hypothesis. Schizophr Res. 2018;194:78-85.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of citalopram on hippocampal volume in first-episode schizophrenia: Structural MRI results from the DECIFER trial. Psychiatry Res Neuroimaging. 2021;312:111286.
- [CrossRef] [PubMed] [Google Scholar]
- Schizophrenia, depressive symptoms, and antipsychotic drug treatment. Int J Neuropsychopharmacol. 2021;24:253-5.
- [CrossRef] [PubMed] [Google Scholar]
- The pharmacologic treatment of schizophrenia-2021. JAMA. 2021;325:175-6.
- [CrossRef] [Google Scholar]
- Current perspectives in treating negative symptoms of schizophrenia: A narrative review (review) Exp Ther Med. 2021;21:276.
- [CrossRef] [PubMed] [Google Scholar]
- May selective serotonin reuptake inhibitors (SSRIs) provide some benefit for the treatment of schizophrenia? Expert Opin Pharmacother. 2016;17:1375-85.
- [CrossRef] [PubMed] [Google Scholar]
- Escitalopram augmentation improves negative symptoms of treatment resistant schizophrenia patients a randomized controlled trial. Neurosci Lett. 2018;681:68-72.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of negative and affective symptoms on anhedonia self-report in schizophrenia. Compr Psychiatry. 2020;98:152165.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical utility of the calgary depression scale for schizophrenia in individuals at ultra-high risk of psychosis. Schizophr Res. 2018;193:423-7.
- [CrossRef] [PubMed] [Google Scholar]
- The Persian version of the calgary depression scale for schizophrenia (CDSS-P) Asian J Psychiatry. 2019;45:44-9.
- [CrossRef] [PubMed] [Google Scholar]
- Escitalopram in the treatment of patients with schizophrenia and obsessive-compulsive disorder: An open-label, prospective study. Int Clin Psychopharmacol. 2013;28:96-8.
- [CrossRef] [PubMed] [Google Scholar]
- Risperidone and escitalopram co-administration: A potential treatment of schizophrenia symptoms with less side effects. Pharmacol Rep. 2017;69:13-21.
- [CrossRef] [PubMed] [Google Scholar]
- Augmentation by escitalopram, but not citalopram or R-citalopram, of the effects of low-dose risperidone: Behavioral, biochemical, and electrophysiological evidence. Synapse. 2012;66:277-90.
- [CrossRef] [PubMed] [Google Scholar]
- No effects of antidepressants on negative symptoms in schizophrenia. J Clin Psychopharmacol. 2013;33:686-90.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of depression in schizophrenia: Systematic review and meta-analysis. Br J Psychiatry. 2017;211:198-204.
- [CrossRef] [PubMed] [Google Scholar]







