Sir,
A 35-year-old female presented with acute abdominal pain in the epigastric and left hypochondriac region since last three days. She also reported associated vomiting and fever. She initially went to a general practitioner where she was diagnosed as having colitis with the help of ultrasonography abdomen. She did not improve with routine medication. Therefore, she was referred to us and we ordered routine blood investigations. She is nondiabetic, and her thyroid profile was standard. Her family and personal history for hyperlipidemia were non-significant. Her BMI was 25 kg/m2. At the outset, we did not suspect pancreatitis as the pain was not typical of pancreatitis and we had ultrasound diagnosis of colitis. Serum became lipemic after 10 min of collection (Figure 1).
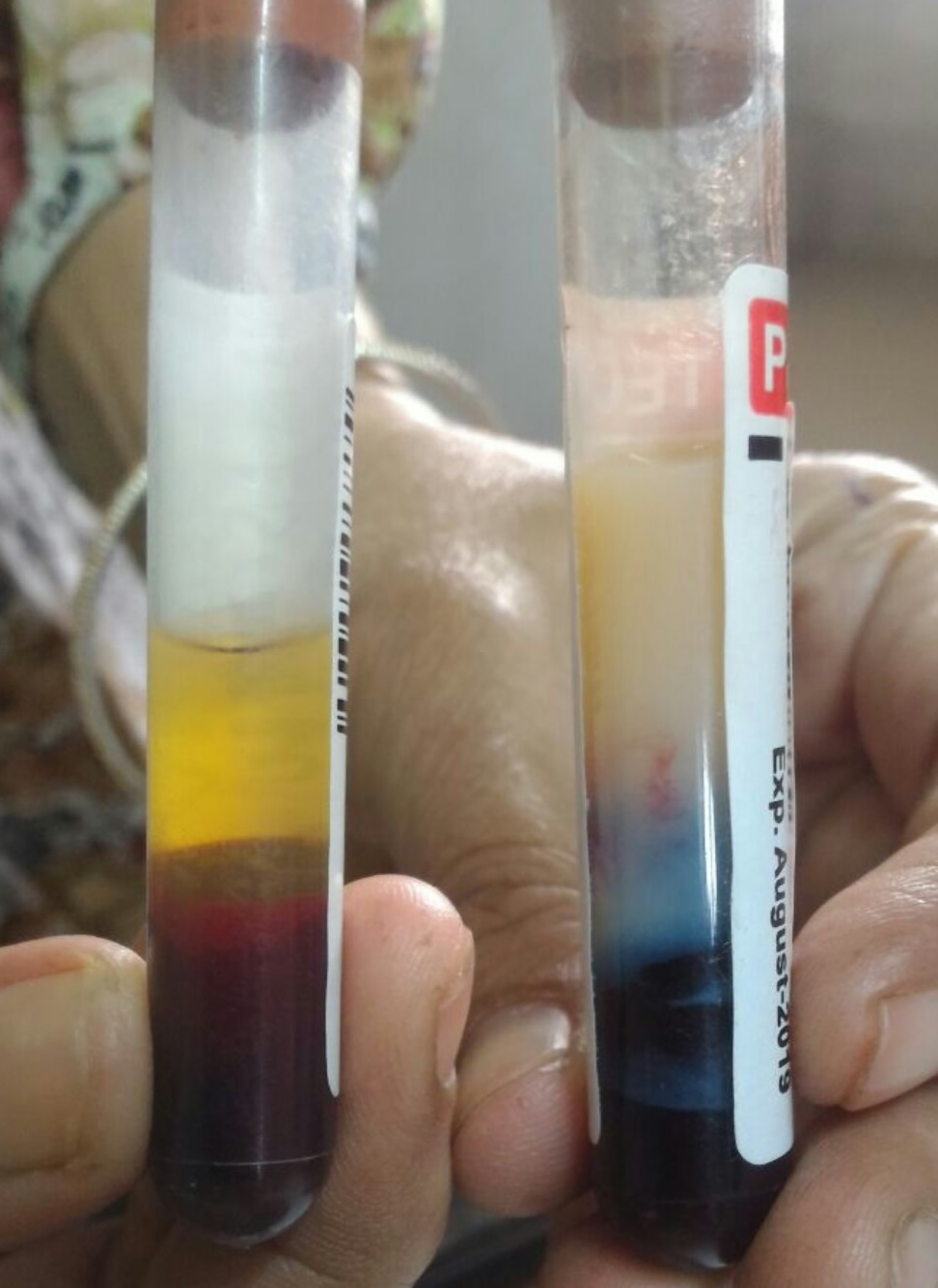
Prompt diagnosis of acute pancreatitis came to our mind. We ordered further investigations to rule out hyperlipidemia and pancreatitis. Her serum amylase was 350 IU/L, lipase 3800U/L, serum cholesterol 835mg/dL and, serum triglyceride 958mg/dL. Diagnosis of acute pancreatitis secondary to hypertriglyceridemia was made. We ordered computed tomography of the abdomen, which confirmed the diagnosis of pancreatitis. She was treated with conservative management and discharged on the 5th day of hospitalization in good health. She was started on lipid-lowering agents (statins). She is on regular follow up since last six months without recurrence, and her lipid profile is within the normal range at present.
Hyperlipidemia is an uncommon cause of acute pancreatitis and accounts for 2 to 5% cases1. Serum triglycerides (TGs) level >500 mg/dl increase the risk of acute pancreatitis2. However, the risk increases with increase in TGs level [>1000 mg/dL (5%) and >2000 mg/dL (10%)]2. Although the mechanisms involved in the pathogenesis of acute pancreatitis secondary to hypertriglyceridemia are not entirely understood, the release of large amounts of fatty acids by lipase inhibited mitochondrial complexes I and V and decreased ATP levels in acinar cells, which induced mitochondrial toxicity in pancreatic acinar cells are implicated3. The endothelial lining of small pancreatic blood vessels is the first target of the injury4. Therefore, Angiopoietin-2 has been recently proposed as a marker of severity in acute pancreatitis5. Free fatty acids can directly injure the membrane by inducing free radical damage1. Hyperlipidemic pancreatitis may be associated with average serum amylase level but elevated serum lipase as in our case4. Suppression of amylase activity by lipemic serum or a non-lipid factor in the circulation is responsible for normal amylase level in hyperlipidemic pancreatitis6,7. The clinical features are similar to pancreatitis associated with other etiologies. Treatment is usually supportive care. Sometimes patients with severe hypertriglyceridemia (>10,000 mg/dl) may be benefited by Plasmapheresis to reduce circulating TGs levels4. Once patients recover, low-fat diet forms the mainstay of therapy4. Antihyperlipidemic agents may be indicated in some cases1. Plasmapheresis lowers the TGs level in the setting of hyperlipidemic pancreatitis, but it does not affect the overall morbidity and mortality8. Gene therapy is a novel target treatment for hyperlipidemic pancreatitis secondary to the specific genetic mutation8.
REFERENCES
- Tenner S, Steinber WM. Acute pancreatitis. In, Feldman M, Friedman LS, Brandt LJ, editors. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. Philadelphia, PA: Elsevier Saunders, 2016;969-93.
- Scherer J, Singh V.P, Pitchumoni CS, et al. Issues in hypertriglyceridemic pancreatitis: An update. J Clin Gastroenterol. 2014;48:195-203.
- Navina, S, Acharya, C, DeLany JP, et al. Lipotoxicity causes multisystem organ failure and exacerbates acute pancreatitis in obesity. Sci Transl Med. 2011;3:107-10.
- Topazian M, Pandol SJ: Acute pancreatitis. In, Yamada T, Alpers DH, Kalloo AN, Kaplowitz N, Owyang C, Powell DW (editors).Textbook of Gastroenterology. West Sussex, UK: Wiley Blackwell; 2009.
- Dumnicka P, Kuśnierz-Cabala B, Sporek M, et al. Serum concentrations of angiopoietin-2 and soluble fms-like tyrosine kinase 1 (sFlt-1) are associated with coagulopathy among patients with acute pancreatitis. Int J Mol Sci. 2017;18(4). pii: E753.
- Clavien PA, Robert J, Meyer P, et al. Acute pancreatitis and normoamylasemia. Not an uncommon combination. Ann Surg. 1989;210:614-20.
- Jap TS, Jenq SF, Wu YC, et al. Mutations in the lipoprotein lipase gene as a cause of hypertriglyceridemia and pancreatitis in 169 Taiwan. Pancreas. 2003;27:122-6.
- Adiamah A, Psaltis E, Crook M, Lobo DN. A systematic review of the epidemiology, pathophysiology and current management of hyperlipidaemic pancreatitis. Clin Nutr. 2017; pii: S0261-5614(17)31360-2.
Vipul Yagnik
Email: vipulyagnik78@gmail.com