INTRODUCTION
The delivery of adequate and safe oxygen therapy to acutely ill medical patients presents many difficulties. In this study we recorded oxygen saturation (SaO2) continuously over prolonged periods by pulse oximetry in order to assess the efficacy of oxygen therapy on an acute medical admitting ward. Pulse oximetry provides estimates of arterial oxyhemoglobin saturation (SaO2) by utilizing selected wavelengths of light to noninvasively determine the saturation of oxyhemoglobin (SaO2) [1, 2]. Various circumstances may affect the accuracy of results. In general, pulse oximetry is useful only in normotensive patients. Those with low flow states or those in shock often have poor peripheral perfusion, resulting in low tissue hemoglobin saturation and falsely depressed pulse oximetry readings [3, 4].
The primary utilities of the pulse oximeter are to determine the relative severity of cardiopulmonary or airway disease, monitor the effectiveness of therapy and monitor for deterioration in condition [5-7].
METHODOLOGY
The present study was conducted with 30 patients on oxygen. They had been admitted to the acute admissions unit over a 3 month period from January 2004 to March 2004. The patients ware randomly selected at different times of the day. They were put on the pulse oximeter (Figure 1) for varying lengths of time (12- 26 hours). The study was independent of Medical management, so recordings did not result in adjustment of therapy.
 |
 |
 |
 |
||
Figure 1: Pulse Oximeter and Recording |
||
To understand how a pulse oximeter is used, it is important to understand how it operates. The oxygen saturation is estimated by measuring the transmission of light through the pulsatile tissue bed [8, 9]. This is based on the Beer-Lambert law [9].
Beer-Lambert law
Beer's law: The intensity of transmitted light decreases exponentially as the concentration of the substance increases. Beer's Law is given by A=ln(Io/I):
 |
Where A is the absorbance - how much light is absorbed while passing through the filter, I is the intensity of light transmitted and Io is the original intensity of light before passing through the filter.
Lambert's law: The intensity of transmitted light decreases exponentially as the distance travelled through the substance increases. The light absorbed by non-pulsatile tissues is constant (DC). The non-constant absorption (AC) is the result of pulsatile blood pulsations. The photo detector generates a voltage proportional to the transmitted light. The AC component of the wave accounts for between 1-5% of the total signal. The high frequency of the diodes allows the absorption to be calculated many times per second. This reduces movement effects on the signal. The microprocessor analyses both the DC and AC components at 660 nm and 940 nm. The absorption of oxyhaemoglobin and deoxyhaemoglobin at these two wavelengths is very different. Hence, these two wave lengths provide good sensitivity.
Isobestic point
This is the point at which two substances absorb a certain wavelength of light to the same extent. In oximetry, the isobestic points of oxyhaemoglobin and deoxyhaemoglobin occur at 590 nm and 805 nm. These points may be used as reference points where light absorption is independent of the degree of saturation. Some earlier oximeters corrected for haemoglobin concentration using the wavelength at the isobestic points. Thus comparison of absorbencies at different wavelengths allows estimation of the relative concentrations of HbO and Hb (i.e. saturation). Modern pulse oximeters may use two or more wavelengths, not necessarily including an isobestic point (Figure 2).
 |
Figure 2: Absorbencies at different wavelengths |
RESULTS
The age of the patients ranged from 25- 85 years with a mean age of 68 years. Majority of cases (i.e. 50%) belonged to the group of chronic obstructive pulmonary disease (Figure 3).
 |
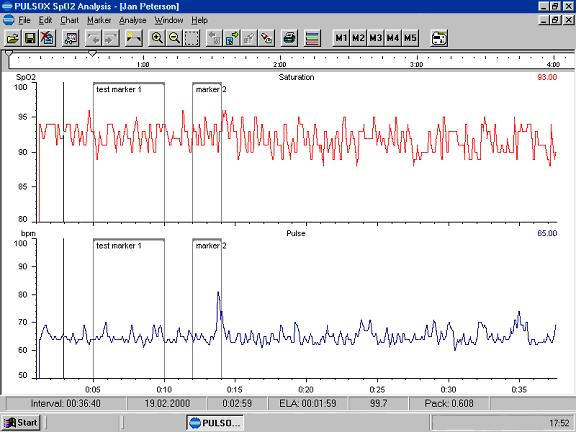
The monitoring of SaO2 was for 12- 26 hours (mean of 18 hours). Oxygen therapy was initiated by doctors in 53% of cases and by nurses in 47% of cases. In all patients SaO2 was monitored 1- 4 hourly but despite this significant hypoxia was common.
- 81% of patients spent more than 1 h at SaO2 less than 85%.
- 26% spent more than 50% of time at SaO2 less than 85%.
- 60% of patients spent a total of 12 hours at SaO2 less than 70%.
- In 43% of patients mean SaO2 was 90% or less.
DISCUSSION
There were two aspects to this study. One was the use of a pulse oximeter for continuous oxygen monitoring to assess the adequacy of oxygen therapy in an acute medical unit. The second was that while oxygen is administered as a matter of routine its dosing may not be adjusted as per requirement. A facility policy may dictate that nurses should notify physicians for pulse oximetry readings below 92%. But if the patient remains stable or continues to improve (or customarily has a lower pulse oximetry result), they may not need to report individual readings immediately. Instead, as with blood sugars, report the aggregate results collected over a day or two, along with other information about the patient's status, including vital signs and results of listening to the lungs, observing and describing respirations, and evaluating the patient overall [10]. In this way, the physician can adjust oxygen administration based on the whole picture.
Physicians should be cautious and realistic about their orders for adjusting oxygen flow to maintain a specific pulse oximetry reading. While oxygen adjustment may be indicated, it may be difficult if not impossible for staff to follow an order, such as; "adjust oxygen to maintain pulse oximetry above 92%." This does not clarify the frequency of monitoring and offers no clue as to the oxygen saturation in between pulse oximetry checks. The best approach may be to monitor the patient's symptoms and physical findings [5].
In patients with known or suspected heart or lung disease, such as chronic obstructive pulmonary disease, the pulse oximetry results may fluctuate and the oxygen saturation may fall or persist below 90%. But one should avoid using the pulse oximetry result alone to determine the urgency of the situation or the need for hospitalization. The patient's overall status and stability of vital signs may be a more important indicator than the fluctuating pulse oximetry results or the difficulty of maintaining a SaO2 above 90%. Although pulse oximetry can be used to gauge the presence of an exercise-induced drop in oxygen saturation in individuals with COPD, no evidence supports using the results to adjust treatments in acute exacerbations of this disease. [11]
In all cases, but especially when SaO2 indicates a possible problem, a nurse, respiratory therapist, or health-care practitioner should evaluate the patient and take accurate, complete vital signs [5]. The presence of stable vital signs, a lack of dyspnea, and a respiratory rate below 28 to 30 indicate the patient may be compensating adequately for hypoxia. Hospitalization may not benefit a patient more than basic care in the long-term care facility [2].
PaO2 can fall to 8kPa with hemoglobin still over 90% saturated. But with a drop from 8 to 5.3kPa, saturation falls steeply to below 75%. Clinically this relationship explains a fundamental goal in treating hypoxemia to get the PaO2 above 8kPa (the flat portion of the curve) [1].
Staff should be aware of factors that may influence pulse oximetry results, including motion artifact, abnormal hemoglobins, exposure of the measuring probe to ambient light during measurement, low perfusion states (including hypotension and shock), skin pigmentation, skin temperature of extremities used to conduct the test, and nail polish or nail coverings with finger probe [9].
CONCLUSION AND RECOMMENDATIONS
There have not been many studies of a similar nature in the literature. Oxygen is a lifesaving drug like any other of a similar kind and should be used judiciously. It should be prescribed and the dose adjustments made like any other medication.
Additionally, documentation should include the date and time of measurement; the pulse oximeter reading; the patient's position, activity level, and location during monitoring; inspired oxygen concentration or supplemental oxygen flow; and the type of oxygen delivery device.
Only properly trained staff should use, document or report pulse oximetry results. One should realize that while hypoxia can kill injudicious, overuse can also be lethal. This is what makes monitoring so very important. We hope our small study will lead to greater consciousness regarding oxygen monitoring in a busy acute medical unit.
REFERENCES
-
Bordow RA, Moser KM. Evaluation of arterial blood gases and acid-base homeostasis. Man Clin Probl Pulm Med. MAXX: The Electronic Library of Medicine [on CD-ROM]. New York, NY: Lippincott, Williams and Wilkins; 1998.
-
Eichhorn JH. Pulse oximetry monitoring and late postoperative hypoxemia on the general care floor. J Clin Monit. 1997;14:49-55.
-
Kaye KS, Stalam M, Shershen WE, et al. Utility of pulse oximetry in diagnosing pneumonia in nursing home residents. Am J Med Sci. 2002;324(5):237-42.
-
Ralston AC, Webb RK, Runciman WB. Potential errors in pulse oximetry. I. Pulse oximeter evaluation. Anaesthesia 1991;46:202-6.
-
Carone M, Patessio A, Appendini L, et al. Comparison of invasive and noninvasive saturation monitoring in prescribing oxygen during exercise in COPD patients. Eur Respir J. 1997;10(2):446-51.
-
Smatlak P, Knebel AR. Clinical evaluation of noninvasive monitoring of oxygen saturation in critically ill patients. Am J Crit Care. 1998;7(5):370-3.
-
Mower WR, Sachs C, Nicklin EL, et al. Effect of routine emergency department triage pulse oximetry screening on medical management. Chest. 1995;108:1297-302.
-
Bowton DL, Scuderi PE, Haponik EF. The incidence and effect on outcome of hypoxemia in hospitalized medical patients. Am J Med. 1994;97:38-46.
-
Wukitisch MW, Peterson MT, Tobler DR, et al. Pulse oximetry: analysis of theory, technology, and practice. J Clin Monit. 1988;4:290-301.
-
Stoneham MD, Saville GM, Wilson IH. Knowledge about pulse oximetry among medical and nursing staff. Lancet. 1994;344:1339-42.
-
Zeballos RJ, Weisman IM. Reliability of noninvasive oximetry in black subjects during exercise and hypoxia. Am Rev Respir Dis. 1991;144:1240-44.