INTRODUCTION
A variety of cardiac and non-cardiac abnormalities have been described following low voltage (<1000 volts) alternate current household (220-240 volts) electric shock [1]. Among cardiac abnormalities, most lethal is sudden death owing to asystole or ventricular fibrillation. Electrocardiogram may show tachycardia, ST-segment changes, arrhythmias, rarely bundle branch block or complete heart block. Infrequently, acute infarction is also noted [2].
CASE REPORT
A 45-year-old man sustained electric current injury on a rainy day, when by mistake the hand held iron rod fell on a live naked road-side high tension electric wire. He noticed loss of movement of left foot and pain in left hip but no angina. Local examination revealed 5cm X 3cm transversely placed linear white, swollen marks in both palms and a charred ulcer 4 cm X 5 cm with raw necrotic base, black rolled out margin on left foot and toes (Figure 1). The systemic examination and vitals were normal. Biochemistry and hemogram were normal except raised creatinine phosphokinase and creatinine phosphokinase myocardium-bound 4567 IU/ml and 14 IU/ml respectively. Electrocardiogram (Figure 2) showed ST elevation and T inversion in C1-C5. Echocardiogram showed left ventricular septal hypokinesia and anteroseptal infarction. He was observed and treated conservatively with aspirin, enoxaparin, β-blocker and alprazolam.
 |
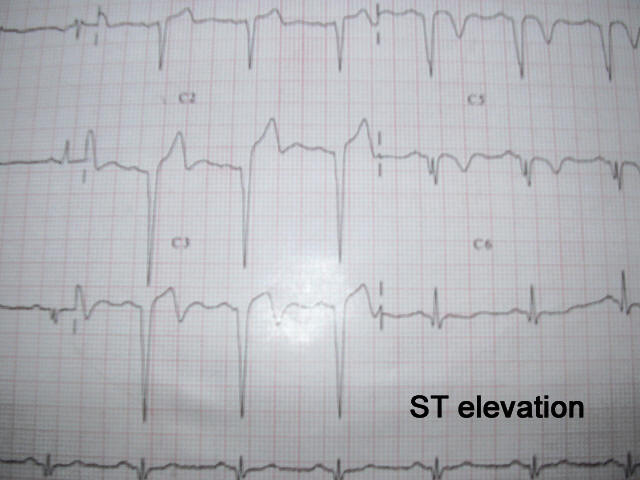 |
Figure 1: Entry and exit wound |
Fig 2: Anterior wall ST elevation and T inversion |
DISCUSSION
Electric current induced tissue damage depends upon amount of electric energy, duration of current, resistance offered by skin and the pathway of electric current [3]. Cardiac tissue is damaged directly by the passage of electric current and indirect damage is caused by altered serum potassium. Initially, there is hyperkalaemia owing to necrosed myocardium. In 2nd to 4th week, there is idiopathic hypokalaemic arrhythmia. Patients should therefore be closely observed for 4 weeks [4].
The structural cardiac damage is localized necrosis and persists for weeks. It manifests as ST elevation and raised cardiac enzymes. The altered functions of myocardium due to changed cell membrane permeability by electric current persist for a short period. Victims of low voltage electric current frequently develop ventricular fibrillation which requires immediate defibrillation [5].
The pathogenesis of electric current induced infarction is controversial. Besides damaging the coronary walls, it also has a direct thrombogenic effect. In the present case, this appears to be a possible mechanism in which myocardial lesions corresponded to acute occlusion of left anterior descending artery perhaps favored by presence of an atheromatous plaque. Here coronary arteriography would have been the most useful investigation.
Population studies suggest that many (20-60%) nonfatal infarctions, passed unrecognized by patients and are discovered only on routine electrocardiogram. Of these infarctions, half are truly silent as patients are unable to recall angina. The other half can recall angina when leading questions are posed [6]. Silent infarctions usually occur in elderly, hypertensive and diabetics without any antecedent angina.
According to Cohen silent infarction patients are having defective anginal warning system [7]. Maseri has proposed that silent ischemia results from a combination of decreased sensitivity to painful stimuli and coronary microvasculature dysfunction [8]. There are many hypotheses to explain this type of silent or painless infarction e.g., abnormal autonomic neuropathy of diabetics, higher than normal pain threshold and lower reaction in elderly hypertensive, individual variation of higher pain threshold for different types of pain stimuli and variable levels of pain threshold-riser endogenous opioids and endomorphins.
CONCLUSION
We infer that this type of silent infarctions occur rarely by electric current due to negligent handling of high tension live wires causing unexpected death. Secondly, local electrical department may be accountable for installing such road side electrical wires near residential places. Thirdly, attending doctors should observe such patients critically before instituting costly and unnecessary thrombolytics.
REFERENCES
-
Raphael C Lee. Electrical Injuries. Braunwald E, Fauci A S, Dennis L Kasper, Stephen L Hauser, Dan L Longo, J Larry Jameson Eds. Harrison's Principles of Internal Medicine. 15th ed. New York: McGraw Hill 2001;393:2583-84.
-
Lewin RF, Arditti A, Sclarovsky S. Non-invasive evaluation of electrical cardiac injury. Br Heart J 1983;49:190-2.
-
Hanson GL, Mollwraith GR. Lightening injury: two case histories and review of management. Br Med J 1973;4:271.
-
Subramanian N, Somasundram B, Periasamy JK. Cardiac injury due to lightening. Indian Heart J 1985;37:72-74.
-
Hampton JR. Chest pain. Warrel PA, Cox TM, Firth JD, Benz jr. JE (eds). Oxford Text Book of Medicine. 4th edition. vol.2. Oxford University Press. New York 2003;829-832.
-
Andrews CJ. Electric shock and lightning Strike. In: Pearn J, ed. The science of first aid. St John’s Ambulance Press. Canberra 1996.
-
Cohn PF. Silent myocardial ischemia: Classification, prevalence, and prognosis. Am J Med 1985 Sep;79(3A):2-6.
-
Mesari A. Ischaemic heart disease. A Rational basis for clinical practice and clinical research. New York. Churchill Livingstone 1995.