Sir,
Proper death certification begins with a fundamental understanding of the cause and manner of death. [1] During the process of medical certification of the cause of death, it is incorrect to write “heart failure,” “cardiac failure,” “cardiopulmonary arrest”, “respiratory arrest” and “brain death” without mentioning the underlying pathological cause. It should be remembered that every death which occurs due to one or the other cause amongst cardio-respiratory failure, cardiac failure, respiratory failure means simply the cessation of circulation and respiration leading to somatic and cellular death. [2] The data on cause of death contained in the certificate serves many purposes, such as assessing the effectiveness of public health programs, providing a feed-back for future policy and implementation, better health planning and management, and deciding priorities of health and medical research programmes. [3] Medical certification of the cause of death by a registered medical practitioner is very important and vital part of his profession. He should have the knowledge of the underlying cause of death of his patient which initiated the train of morbid events leading directly to death; and certification of cause of death. The cause of death must be properly determined before lawful disposal of the dead body. In cases where the cause of death is unknown, body should be subjected for medico-legal or pathological (clinical) autopsy to ascertain the cause of death depending upon the circumstances. This will fulfill the requirements of International Classification of Diseases (ICD) developed by WHO (10th revision) when death certificates are issued. This article is aimed to sensitize the registered medical practitioners about the importance of medical certification of cause of death and to improve recording of the cause of death.
A cause of death is a disease, abnormality, injury or poisoning that contributes directly or indirectly to death. A death often results from the combined effects of two or more conditions. These conditions may be completely unrelated, arising independently of each other; or casually related to each other. The underlying cause i.e. the disease or injury which has initiated the sequence of events will get selected for the purpose of tabulation. These morbid conditions or injuries consequent to the underlying cause relating to death are termed as antecedent and immediate cause. [3] According to the legal provisions made in the Registration of Births and Deaths Act, 1969 (18 of 1969), the certification of the cause of death by a medical practitioner who has attended the deceased during the latter’s last illness is necessary. A certificate as to the cause of death shall be obtained in the event of death of any person who, during his illness was attended by a medical practitioner, the medical practitioner shall, after the death of that person, forth with, issue without charging any fee, to the person required under this Act to give information concerning the death, a certificate in the prescribed form stating to the best of his knowledge and belief the causes of death; and the certificate shall be received and delivered by such person to the registrar at the time of giving information concerning the death as required by this Act. [4] According to section 17(2) of the Registration of Births and Deaths Act, 1969, all extracts given under this Act shall be certified by the registrar or any other officer authorized by the State Government to give such extracts as provided in section 76 of the Indian Evidence Act, 1872 (1 of 1872), and shall be admissible in evidence for the purpose of proving the birth or death to which the entry relates. [4]
As per provisions laid down by the Indian Medical Council (Professional conduct, Etiquette and Ethics) Regulations, 2002, certificates are issued by doctors for the purpose of the Acts relating to birth, death or disposal of the dead. [5] The registered medical practitioner’s primary responsibility is to complete the medical part of the certificate regarding all diseases, morbid conditions or injuries which either resulted in or contributed to death.
he attending doctor should have complete knowledge about the disease or injury which initiates the chain of events ultimately leading to the cause of death. If untimely deaths are to be prevented the chain of events has to be cut or cure instituted at some intermediate point. The most effective public health objective is to prevent the precipitating cause from operating and hence the relevance of the underlying cause. The medical part of the certificate should normally be the responsibility of the attending medical practitioner and based on his individual assessment. In cases of suspicious, unnatural deaths and other medico-legal cases in which medico-legal autopsy is indicated, the last attending medical practitioner should not issue the “death certificate,”. The case should be informed to the police and the dead body should be kept in safe custody till it is forwarded for medico-legal autopsy by the inquest concerned. The fact of death in such cases should however, be communicated to the local registrar in the prescribed format pending the final filling up and transmission of the medical certificate to the registrar concerned. The death certificate may later be issued by the registrar of Births and Deaths. [3] The standard format of the certificate is incorporated in the rules made by the Indian Government. Form No. 4 is used as medical certificate of cause of death for hospital in-patients deaths and is to be sent to registrar. [3]
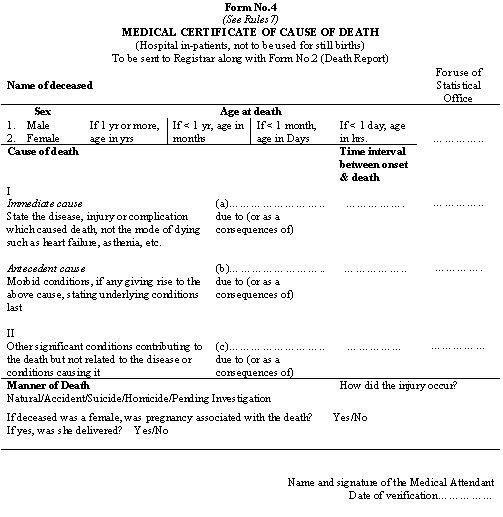 |
The medical part of the certificate is designed by the WHO to facilitate reporting the underlying cause of death and to obtain information of the casual and pathological sequence of events leading to death. It consists of two parts, the first relating to the sequence of events leading to death, and the second to other significant conditions that contributed to the death. This part should be written by the attending medical practitioner having personal knowledge of the case history. The name of the disease should be written in full and legibly to avoid the risk of their being misread. Abbreviations and short form of disease condition should not be used. Only one cause is to be entered on each line of Part I. The underlying cause of death (the condition that started the sequence of events between normal health and the direct or immediate cause of death) should be entered on the lowest line used in this part. The followings are some examples of immediate and antecedent causes of death:
Clinical causes
-
The death was due to myocardial infarction as a result of coronary arterial occlusion as a consequence of atherosclerosis.
-
The death was due to peritonitis as a result of perforation as a consequence of duodenal ulcer.
-
The death was due to chronic renal failure as a result of hypertension as a consequence of polycystic kidney disease.
-
The death was due to uraemia as a result of retention of urine as a consequence of hyperplasia of the prostate.
-
The death was due to emaciation as a result of metastasis to lymph nodes and liver as a consequence of bronchogenic carcinoma of right lung.
Medico-legal causes
-
The death was due to asphyxia as a result of constriction of neck as a consequence of hanging or strangulation.
-
The death was due to cerebral ischemia as a result of occlusion of carotid arteries as a consequence of throttling.
-
The death was due to asphyxia as a result of aspiration of fluid in air passages as a consequence of wet drowning.
-
The death was due to shock and hemorrhage as a result of rupture of spleen as a consequence of blunt injury to left hypochondriac region.
-
The death was due to shock and hemorrhage as a result of fracture of middle cranial fossa as a consequence of head injury.
Registered medical practitioners are expected to have complete knowledge of the sequence of events of underlying cause which may lead to death. They should fulfill the requirement of International Classification of Diseases developed by WHO (10th revision) to comply within form 4 in respect of all institutional deaths in government and private hospitals and all domiciliary deaths. In cases where the cause of death is not known or could not be ascertained, the dead body should be subjected for autopsy to determine the cause of death which provides authentic data for better health care planning and management, and vital statistics. There is need for active involvement and co-operation of the doctors to make the scheme successful on medical certification of cause of death, formulated by the office of the Registrar General, India. This scheme should be expanded to all medical colleges, hospitals and primary health centers. Indian Medical Association and other medical organizations like National Medicos Organization, etc. may participate in this scheme on medical certification of cause of death to make it successful. There is need to sensitize the registered medical practitioners about the importance of the medical certification into the cause of death and come forward in improving the recording of cause of death.
REFERENCES
-
Dolinak D, Matshes EW, Lew EO. Forensic Pathology: Principles and Practice. Elsevier Academic Press 2005:663.
-
Mathiharan K, Patnaik AK. Modi’s Medical Jurisprudence and Toxicology. 23rd edition. Lexis Nexis, New Delhi 2006: 241.
-
Physician’s Manual on Medical Certification of Cause of Death. 4th Edition. Vital Statistics Division, Office of the Registrar General, India, Ministry of Home Affairs, New Delhi 2000.
-
The Registration of Births and Deaths Act, 1969 (18 of 1969). Universal Law Publishing Co. Pvt. Ltd, Delhi 2006: 6-8.
-
The Indian Medical Council (Professional conduct, Etiquette and Ethics) Regulations. Notification No. MCI 211(2) 2001. The Gazette of India 2002.
Dr. P C Srivastava MD
Assistant Professor
Department of Forensic Medicine
Email: premshikha1115@rediffmail.com